December 2021
The impact of the COVID-19 pandemic on Americans’ physical health and economic security is evident. New data shows other significant impacts, like disruption of mental and behavioral healthcare, continued alarming increases in drug overdoses, more suicide attempts among adolescents, and divergent trends in suicide rates.
In May of 2021 TFAH and Well Being Trust’s Pain in the Nation report described emerging data on many of COVID-19’s direct and indirect effects related to mental health and substance use, including more calls to crisis lines, worse reported mental health, more substance use, and higher rates of drug overdoses. Additional data and studies released in 2021 show a more complete picture of the effects of the pandemic on mental and behavioral healthcare, drug overdoses, and suicidal behaviors. Here’s what we’ve learned from four new studies:
Reduced utilization of mental and behavioral healthcare in 2020
A February 2021 report from Milliman examined utilization patterns for mental health and substance use healthcare for 12.5 million Americans with health coverage from private health plans, Medicaid, and Medicare between January 2019 and August 2020. The authors found that in-person mental and substance use services declined substantially in early 2020 at the beginning of the pandemic. This includes decreases in inpatient admissions, emergency services, primary care visits, and specialty care visits for mental and behavioral healthcare. The largest declines were in-person primary care and specialty care visits in April, May, and June 2020—these visits declined 75 percent for individuals with private health coverage. In June 2020, utilization began to increase until it reached or surpassed 2019 levels by the end of the summer.
The report also looked at telehealth visits, which increased dramatically in March and April, particularly for individuals with private plans and Medicare. In prior years, 1 percent or less of mental or behavioral healthcare visits were via telehealth, while it exceeded 75 percent for private plan enrollees and 50 percent for Medicare enrollees at the peak. For Medicaid enrollees, the uptake was much lower—peaking at 28 percent for Medicaid enrollees—pointing to limitations of telehealth to reach all patients.
Continued increase in drug overdoses in 2020–2021
Provisional data from the CDC shows a rapid escalation in drug overdose deaths since the beginning of 2020 after several years of relatively flat death rates. The most recent data released—for the 12-month period May 2020–April 2021—shows 97,990 provisional drug overdose deaths. In comparison, a year prior (May 2019–April 2020), had 77,007 provisional drug overdose deaths and two years prior (May 2018–April 2019), had 67,736 provisional drug overdose deaths. The increases were nearly universal across states with just three states (New Hampshire, New Jersey, and South Dakota) seeing decreases, and several states (Kentucky, Louisiana, Tennessee, Vermont, West Virginia) having staggering increases of more than 50 percent.
More suicide attempts among adolescents during the pandemic
A CDC study from June 2021 compared the number of emergency department visits for suspected suicide attempts for 12–17-year-olds before and during the pandemic. The study found that in May 2020, suspected suicide attempts among adolescents began to increase, particularly among girls, and remained higher through 2021. During the weeks of February 21–March 20, 2021, suspected suicide attempts were 51 percent higher among girls aged 12–17 years than during the same period in 2019; among boys aged 12–17 years, suspected suicide attempts increased 4 percent.
Suicide trends diverge by population groups in 2020
The National Center for Health Statistics released a report using provisional mortality data to examine suicide trends in 2020 in November 2021. The topline trend shows a drop in the overall suicide rate from 13.9 deaths per 100,000 in 2019 to 13.5 deaths per 100,000 in 2020. This includes a notable drop in suicides in April 2020, at the beginning of the pandemic. For the year 2020, suicide rates declined across many groups including for females of all race/ethnicities, middle age adults (aged 35-64), whites, and Asians. There are several major exceptions to this trend: younger Americans (aged 10-34) saw increases in suicide rates between 2019 and 2020— including a statically significant increase among young adults aged 25–34 years old— and likewise American Indian/Alaska Native, Black, and Hispanic males saw increases in suicide rates between 2019 and 2020—including a statistically significant increase for Hispanic males. These divergent trends by age, sex, and race/ethnicity highlight the importance of collecting demographic information and analyzing trends among populations in order understand the different outcomes and experiences, and how best to focus resources and policy responses towards those in need.
Policy action is needed
These new studies underscore the need for urgent action, or risk an increase in deaths from alcohol, drugs, and suicide — already on a grim trajectory—in the coming years.
“The pandemic has created new stressors, and worsened the substance use and mental health crises in our country. We need to focus on how we can better support individuals with emergent crises, mental health conditions, and substance use disorders now, as well as look ahead and invest in policies that promote good health, well-being, equity, and resilience for everyone,” said J. Nadine Gracia, President and CEO Trust for America’s Health.
Specifically, we need to make progress in three priority areas:
Invest in Prevention and Conditions that Promote Health
- Reduce traumatic experiences, and promote resilience in children, families, and communities. Programs that promote economic security, such as a living wage, and create affordable housing help strengthen families and reduce traumatic experiences in childhood.
- Expand substance use prevention, mental health, and resiliency programs and staff in schools.
- Bolster crisis-intervention programs and supports.
- Reduce availability of illicit opioids and inappropriate prescriptions.
- Lower excessive alcohol use through evidence-based policies such as increasing pricing, reducing sales hours and enforcing underage drinking laws.
- Limit access to lethal means of suicide, including drugs and firearms.
Address the Worsening Drug Use and Overdose Crisis
- Implement policies targeting psychostimulant use.
- Promote harm-reduction policies to reduce overdose and blood-borne infections.
- Continue pandemic-related enhanced flexibilities in access to and rules for substance-use treatment.
- Address the secondary impact of the substance use and overdoses on children.
Transform the Mental Health and Substance Use Prevention System
- Expand efforts to combat stigma and improve social attitudes toward mental health.
- Improve data accuracy, completeness, and timeliness through innovation and additional funding.
- Increase access to mental health and substance use healthcare through full enforcement of the Mental Health Parity and Addiction Equity Act.
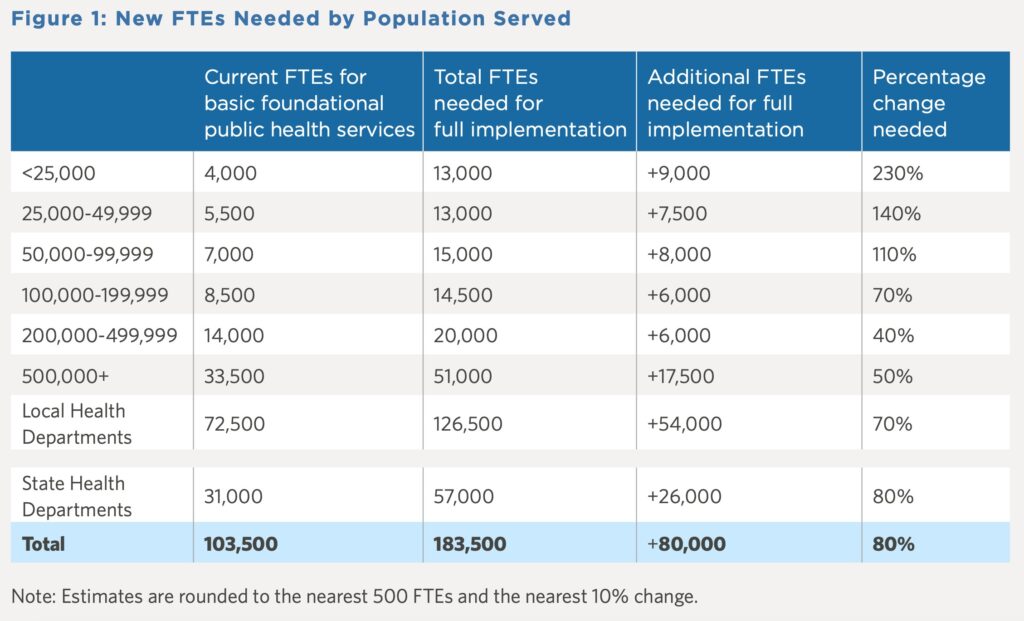
- Expand the mental health and substance use treatment workforce.
- Build community capacity for early identification and intervention for individuals with mental health needs.
- Promote diversity and culturally appropriate care in the healthcare system and adopt trauma-informed and culturally competent practices in youth-services programs.
For more details on these policies, see the solutions and recommendations section in the latest Pain in the Nation report.