The death of three-time Olympian Tori Bowie due to complications from childbirth in 2023 was yet another tragic loss. Her death and that of far too many women highlight the disturbing maternal health crisis in the United States.
Despite having the highest healthcare spending among high-income countries, the United States has the highest maternal mortality rate among those countries. And this maternal health crisis is disproportionately impacting Black women, Native American women, and women in rural areas.
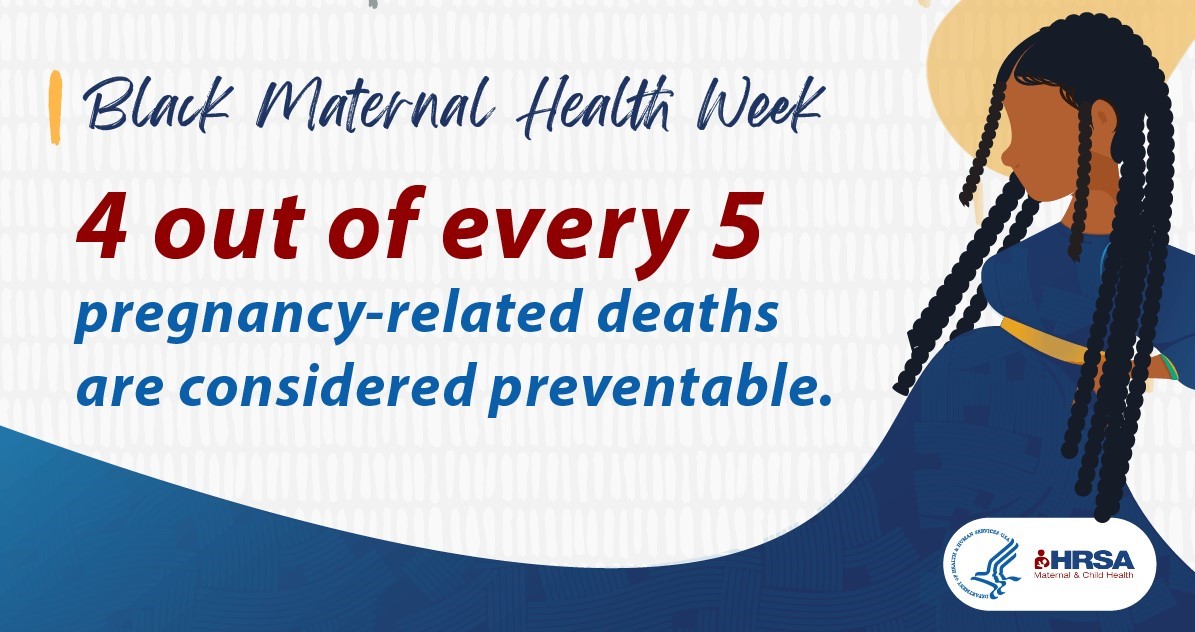
Roughly 700 women in the U.S. die each year from pregnancy-related or childbirth complications, according to the Centers for Disease Control and Prevention. Many of these deaths are preventable. The maternal mortality rate for Black women is almost three times greater than that of white women over the last decade.
Black Maternal Health Week is recognized each year from April 11-17 to bring attention and action improving Black maternal health. It also coincides with April being National Minority Health Month.
The call to take action on Black maternal health has reached the highest levels of the U.S. government. The White House Blueprint for Addressing The Maternal Health Crisis outlines actions the Biden-Harris Administration will take to improve maternal health, all rooted in a focus on health equity. The action steps include increasing access to and coverage of comprehensive high-quality maternal healthcare, advancing data and research on maternal health issues, expanding and diversifying the perinatal workforce, and strengthening economic and social supports for pregnant people and families.
States are also responding with innovative and collaborative solutions that could revolutionize how the country supports expecting mothers.
New Jersey is one such example. The state rolled out a comprehensive plan in 2021 to address maternal health, especially for mothers and babies of color. Nurture New Jersey was launched by the state’s first lady, Tammy Murphy, and was informed by years-long, science-based, multisector planning. The final report includes actionable commitments to build and improve racial equity and community infrastructure, engage multiple public and private sectors to achieve collective impact on health, and strategies to shift narratives and mindsets around maternity.
Murphy initiated an annual Black Maternal and Infant Health Summit, bringing together stakeholders from healthcare, academia, and community-based organizations. The state has made efforts to improve access to midwifery services and to improve the workforce pipeline. And the state issues a maternal health hospital report card that grades every licensed birthing facility to provide residents with another layer of information during their family planning.
New Jersey has the fourth highest maternal mortality rates in the nation with 46 maternal deaths per 100,000 live births, as reported in the Georgetown Institute for Women, Peace and Security’s 2020 U.S. Women, Peace and Security Index. For Black women within the state, that rate rises to 132 deaths per 100,000 live births. The state’s plan calls for reducing maternal mortality rates by 50 percent.
Other states have used targeted strategies to address specific areas of concern.
Forty-six states, including the District of Columbia, have extended Medicaid postpartum coverage from 60 days to 12 months, and two other states are planning to implement a 12 month extension. The American Rescue Plan Act of 2021 gave states the option to extend coverage. More than half of births to individuals of color are covered by Medicaid.
More than half of states allow Medicaid to cover doula services. Many of women of color choose doulas during their pregnancy for more personal support and due to concerns about implicit and explicit bias that exists within the healthcare system.
Other actions states can take to improve maternal care include postpartum coverage extension. To date, numerous states have introduced legislation to extend such coverage and two have succeeded: California and Texas. In addition, states should prioritize Medicaid applications for pregnant people as Hawaii and Rhode Island have done.
By using the governmental, community, and cultural resources such as doulas and midwives to support Black women and families during pregnancy, the U.S. has the opportunity to vastly improve maternal health care and outcomes.