State Category: Oklahoma
TFAH’s Board Chair and President and CEO, Statement in Honor of Martin Luther King, Jr. Day and the National Day of Racial Healing
“Today’s observation of Martin Luther King, Jr. Day and tomorrow’s National Day of Racial Healing are a time to take action to end racism, heal the impacts of centuries of racial injustice, and promote equity for all people.
As the COVID-19 pandemic has demonstrated, long-standing structural racism within our society causes a disproportionate negative impact on people of color, especially during public health emergencies.
TFAH’s goal is to secure the opportunity for optimal health for everyone and make all communities more resilient. This includes advancing policies that promote health and address the primary drivers of health disparities.
We are committed to continuing to support and advocate for policies that overcome the impacts of racism and advance health equity. Meaningful change will require racial healing, which will in turn necessitate acknowledging the historical and contemporary impacts of racism, building meaningful relationships across communities, and policy change.”
Among TFAH’s policy priorities for promoting health equity in 2023 are the following:
Invest in policies and capacity to address the social determinants of health: Congress should fund the Centers for Disease Control and Prevention’s Social Determinants of Health work to enable communities to work across sectors to address the non-medical drivers of poor health outcomes.
Target the elimination of poverty by implementing living wage policies and expanding the Earned Income Tax Credit at the national and state levels.
Strengthen leadership for health equity and incorporate lessons learned from the COVID-19 pandemic into future preparedness and response capabilities. The White House, Congress, and relevant federal, state, local, tribal, and territorial agencies should continue to implement the recommendations of President Biden’s COVID-19 Health Equity Task Force. The White House should create a permanent health equity infrastructure to implement and ensure accountability for these recommendations and bolster equity leadership and coordination for future health crises.
Provide job-protected paid leave. The pandemic called attention to the fact that paid family, sick, and medical leave protect individual’s and families’ economic security and are important infection-control measures. Congress should enact a permanent federal paid family and medical leave policy and dedicated paid sick days protections, including for preventive services such as vaccination.
Congress and federal agencies should ensure federal funding is reaching localities and organizations that represent and serve communities that encounter disproportionate barriers to good health.
Public health agencies should appoint chief health equity officers who would be part of the response, planning, and activation teams for all emergencies.
Increase access to high-quality healthcare for all by strengthening incentives to expand Medicaid and by making marketplace coverage more affordable for people with low- and moderate-incomes.
Increase funding for programs that promote long-term security and good health for children and families, including programs designed to expand access to affordable housing and Head Start, Early Head Start, and nutrition support programs such as Healthy School Meals for All, the Supplemental Nutrition Assistance Program (SNAP), and the Special Supplemental Nutrition Assistance Program for Women, Infants, and Children (WIC).
For more information, see TFAH’s reports.
Trust for America’s Health is a nonprofit, nonpartisan organization that promotes optimal health for every person and community and works to make the prevention of illness and injury a national priority. www.tfah.org
The National Day of Racial Healing, is sponsored by the W.K. Kellogg Foundation. According to the Foundation, the day is a time to contemplate our shared values and create a blueprint for #HowWeHeal from the effects of racism. W.K. Kellogg Foundation (wkkf.org)
Trust for America’s Health is a Healthy People 2030 Champion!
As an organization that prioritizes optimal health for all people, Trust for America’s Health (TFAH) is pleased to be recognized as a Healthy People 2030 Champion by the U.S. Department of Health and Human Services (HHS). TFAH shares the Healthy People 2030 vision of a society in which all people can achieve optimal health and well-being across the lifespan. This commitment is reflected in TFAH’s overall vision and mission and within its Age-Friendly Public Health Systems (AFPHS) initiative. TFAH prioritizes achieving equity in all of our work and promotes optimal well-being for all by focusing on the social determinants of health (SDOH).
TFAH has worked closely HHS leadership, particularly within the Office of Disease Prevention and Health Promotion, which administers Healthy People 2030, to promote stronger collaborations between state departments of health and state aging agencies.
The Age-Friendly Public Health Systems initiative and Healthy People 2030 are well aligned as they share a focus on optimal health in every community. AFPHS’s 6C’s strategy provides a roadmap for state and local health departments to engage in activities that support healthy aging in their communities including:
Connecting and convening multi-sector stakeholders
Coordinating existing supports and services
Collecting, analyzing, and translating relevant data
Communicating important public health information
Complementing existing health promoting programs
Creating and leading policy, systems, and environmental changes
In addition to the Healthy People 2030/AFPHS alignment, TFAH supports the Healthy People 2030 vision in the following ways:
Promoting and increasing access to disease prevention and health promotion activities.
TFAH’s federal advocacy priorities focus on strengthening the public health system so that every state, tribal, local, and territorial health department has the funding and capacity to improve and sustain optimal health for every person and community.
Addressing social determinants of health, eliminating disparities, achieving health equity, and/or promoting well-being.
TFAH is leading advocacy efforts to increase public health’s capacity to fully address the social determinants of health, with a focus on equity and eliminating disparities in health across the lifespan.
Providing training and other necessary resources to adapt or modify disease prevention and health promotion activities to meet the needs of diverse populations, address SDOH, eliminate disparities, achieve health equity, and/or promote well-being.
Many of TFAH’s reports and policy briefs document states where health promotion activities need improvement, as well as feature best practices. In addition, TFAH’s website includes detailed health data on every state and territory including on emergency preparedness, prevalence of chronic diseases and flu vaccination rates.
Developing partnerships across a variety of sectors, including public health, healthcare, government, philanthropy, civil rights, academia, education, community, faith-based, media, business, and technology
TFAH routinely hosts convenings of representatives across sectors including public health, healthcare, government, philanthropy, academia, community, and education. Such convenings have focused on the COVID-19 pandemic, adolescent health, healthy aging, state policies to promote health and control costs, and many other topics.
TFAH looks forward to continuing our strong partnership with the HHS Office of Disease Prevention and Health Promotion and other Healthy People 2030 Champions to create and sustain opportunities for all Americans to live healthfully and productively throughout their lives.
New CDC Data Shows 4 Percent Rise in Suicides in 2021
On September 30, the Centers for Disease Control and Prevention (CDC) released a new report on provisional data on suicide mortality in 2021. The new data shows a 4 percent increase in the national suicide rate—rising from 13.5 deaths per 100,000 population in 2020 to 14.0 deaths per 100,000 population in 2021. In contrast, the national suicide rate declined in both 2019 and 2020, though it had steadily increased over the previous two decades.
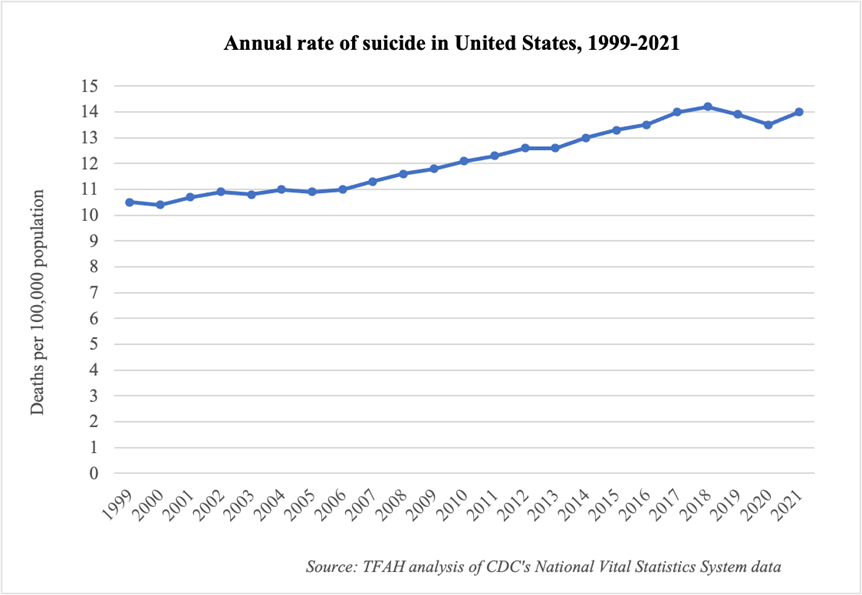
The report also includes additional information on suicide by sex, age group, and month. Key takeaways:
- Suicide rates increased more among males (3 percent increase) than females (2 percent increase).
- Suicide rates increased for people in nearly all age groups. The only exception was a 2 percent decline for people age 75 and over, though it was not a statistically significant change.
- The largest statistically significant increase among all sex/age groups was for males aged 15–24, with an 8 percent increase in suicide rate from 2020 to 2021. Females aged 10–14 had the largest percentage increase in suicide rate (15 percent), though the change was not statistically significant due to a relatively small numbers of cases.
- There were more suicides across all months of 2021 compared with 2020, except in January, February, and July. The largest increase across all the months was an 11 percent increase in suicide rate in October.
The report does not include racial/ethnic or geographic information, nor information on suicide method—all critical pieces to understanding the full picture. For example, data from 2020 showed higher rates of suicide among American Indian, Black, and Latino people and of suicide by firearm—all in a year when the overall suicide rate declined. The National Center for Health Statistics will likely release final 2021 mortality data, including these additional data points, in December.
“The increase in suicide is devastating,” said J. Nadine Gracia, M.D., MSCE, President and CEO of Trust for America’s Health (TFAH). “The new data underscores the need for more attention on this issue and action to prevent future suicides—by federal policymakers, the private and non-profit sectors, and every community across the nation. This study is a wakeup call that we continue to face a mental health and substance use crisis, but we can prevent these tragic deaths.”
The most recent Pain in the Nation report from TFAH includes 2020 data and an analysis of longer-term trends, as well as policy recommendations for reducing alcohol, drug, and suicide deaths. The new CDC report reaffirms the importance of many of these recommendations, including to:
- Strengthen the continuum of crisis intervention programs with a focus on the newly established “988” lifeline.
- Expand CDC’s comprehensive suicide-prevention efforts, including measures to strengthen economic supports, promote connectedness, and create protective environments.
- Address the social determinants of health and promote resilience in children, families, and communities, including through economic supports, access to quality childcare, and prevention and early intervention efforts in schools.
- Build grassroots community capacity for early identification and intervention for individuals with mental health and substance use disorders, including through community-based or non-traditional settings.
- Limit access to lethal means of suicide, including drugs and firearms, among individuals at higher risk of suicide through state and federal laws, more funding of foundational research, and the adoption of counseling programs in healthcare systems.
New CDC Data Shows 4 Percent Rise in Suicides in 2021
On September 30, the Centers for Disease Control and Prevention (CDC) released a new report on provisional data on suicide mortality in 2021. The new data shows a 4 percent increase in the national suicide rate—rising from 13.5 deaths per 100,000 population in 2020 to 14.0 deaths per 100,000 population in 2021. In contrast, the national suicide rate declined in both 2019 and 2020, though it had steadily increased over the previous two decades.
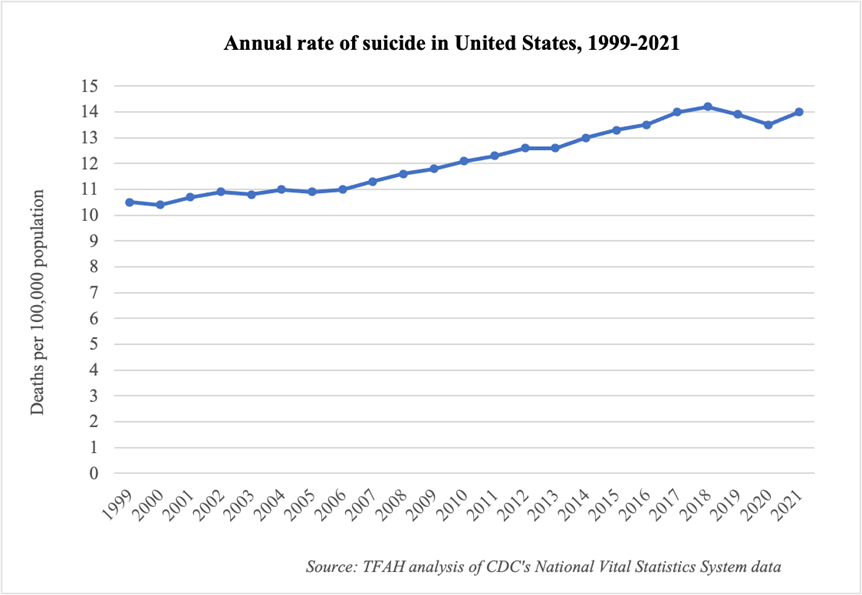
The report also includes additional information on suicide by sex, age group, and month. Key takeaways:
- Suicide rates increased more among males (3 percent increase) than females (2 percent increase).
- Suicide rates increased for people in nearly all age groups. The only exception was a 2 percent decline for people age 75 and over, though it was not a statistically significant change.
- The largest statistically significant increase among all sex/age groups was for males aged 15–24, with an 8 percent increase in suicide rate from 2020 to 2021. Females aged 10–14 had the largest percentage increase in suicide rate (15 percent), though the change was not statistically significant due to a relatively small numbers of cases.
- There were more suicides across all months of 2021 compared with 2020, except in January, February, and July. The largest increase across all the months was an 11 percent increase in suicide rate in October.
The report does not include racial/ethnic or geographic information, nor information on suicide method—all critical pieces to understanding the full picture. For example, data from 2020 showed higher rates of suicide among American Indian, Black, and Latino people and of suicide by firearm—all in a year when the overall suicide rate declined. The National Center for Health Statistics will likely release final 2021 mortality data, including these additional data points, in December.
“The increase in suicide is devastating,” said J. Nadine Gracia, M.D., MSCE, President and CEO of Trust for America’s Health (TFAH). “The new data underscores the need for more attention on this issue and action to prevent future suicides—by federal policymakers, the private and non-profit sectors, and every community across the nation. This study is a wakeup call that we continue to face a mental health and substance use crisis, but we can prevent these tragic deaths.”
The most recent Pain in the Nation report from TFAH includes 2020 data and an analysis of longer-term trends, as well as policy recommendations for reducing alcohol, drug, and suicide deaths. The new CDC report reaffirms the importance of many of these recommendations, including to:
- Strengthen the continuum of crisis intervention programs with a focus on the newly established “988” lifeline.
- Expand CDC’s comprehensive suicide-prevention efforts, including measures to strengthen economic supports, promote connectedness, and create protective environments.
- Address the social determinants of health and promote resilience in children, families, and communities, including through economic supports, access to quality childcare, and prevention and early intervention efforts in schools.
- Build grassroots community capacity for early identification and intervention for individuals with mental health and substance use disorders, including through community-based or non-traditional settings.
- Limit access to lethal means of suicide, including drugs and firearms, among individuals at higher risk of suicide through state and federal laws, more funding of foundational research, and the adoption of counseling programs in healthcare systems.
State of Obesity 2022: Better Policies for a Healthier America
Nation’s Obesity Epidemic is Growing: 19 States Have Adult Obesity Rates Above 35 Percent, Up From 16 States Last Year
Social and Economic Factors Are Key Drivers of Increasing Obesity Rates
(Washington, DC – September 27, 2022) – Four in ten American adults have obesity, and obesity rates continue to climb nationwide and within population groups, according to a report State of Obesity 2022: Better Policies for a Healthier America released today by Trust for America’s Health (TFAH). The report amplifies the importance of the White House Conference on Hunger, Nutrition and Health happening tomorrow. The Conference and the report are intended to spotlight the links between hunger, nutrition, and health, and diet-related diseases including obesity. In addition, they will drive policy action to address food insecurity and health disparities, factors often at the root of diet-related health issues.
The report finds that persistent increases in obesity rates across population groups underscores that obesity is caused by a combination of factors including societal, biological, genetic, and environmental, which are often beyond personal choice. The report’s authors conclude that addressing the obesity crisis will require attending to the economic and structural factors of where and how people live.
Based in part on newly released 2021 data from the Centers for Disease Control and Prevention’s Behavioral Risk Factors Surveillance System, and analysis by TFAH, the report tracks rates of overweight and obesity by age, race/ethnicity, and state of residence. Among the most striking findings are:
Nineteen states have adult obesity rates over 35 percent. West Virginia, Kentucky, and Alabama have the highest rate of adult obesity at 40.6 percent, 40.3 percent, and 39.9 percent, respectively. The District of Columbia, Hawaii, and Colorado had the lowest adult obesity rates at 24.7 percent, 25 percent, and 25.1 percent respectively.
A decade ago, no state had an adult obesity rate at or above 35 percent. (See state-by-state rate chart).
National data from the 2017-2020 National Health and Nutrition Examination Survey also included in the report show the following:
- Nationally, 41.9 percent of adults have obesity.
- Black adults had the highest level of adult obesity at 49.9 percent.
- Hispanic adults had an obesity rate of 45.6 percent.
- White adults had an obesity rate of 41.4 percent.
- Asian adults had an obesity rate of 16.1 percent.
- Rural parts of the country had higher rates of obesity than did urban and suburban areas.
Structural and social determinants are significantly influencing the rates of obesity among adults and youth. Factors such as structural racism, discrimination, poverty, food insecurity, housing instability, and lack of access to quality healthcare are key drivers of the differences in obesity rates across racial and ethnic groups. These systemic barriers make it inappropriate to assign blame to individuals with obesity for their weight. The purpose of this report is to analyze conditions in people’s lives which make them more likely to develop obesity and recommend policies to address those conditions.
Obesity rates are also increasing among children and adolescents with nearly 20 percent of U.S. children ages 2 to 19 having obesity. These rates more than tripled since the mid-1970s and Black and Latino youth have substantially higher rates of obesity than do their white peers.
A special section of the report looks at the relationship between food insecurity and obesity. Food insecurity, defined as being uncertain of having or unable to acquire enough food because of insufficient money or resources, is driven by many of the same social and economic factors that drive obesity including poverty and living in communities with many fast-food establishments but limited or no access to healthy, affordable foods such as available in full-service supermarkets or farmers markets. Being food and nutrition insecure often means families must eat food that costs less but is also high in calories and low in nutritional value.
Obesity is multifactored and involves more than individual behavior
Social and economic factors including experiencing poverty and the impact of long-standing structural racism and health inequities are strongly associated with obesity and are at the root of higher rates of obesity in low-income communities that have fewer resources to support healthy eating and being physically active.
“The continued increase in rates of obesity across all population groups is alarming,” said J. Nadine Gracia, M.D., MSCE, President and CEO of Trust for America’s Health. “Policies and programs to reduce obesity need to be implemented at a systems level. We must advance policies that address the community, institutional, and structural factors that are barriers to healthy eating and physical activity and that exacerbate health inequities.”
Addressing obesity is critical because it is associated with a range of diseases including type 2 diabetes, heart disease, stroke, arthritis, sleep apnea, and some cancers. Obesity is estimated to increase U.S. healthcare spending by $170 billion annually (including billions by Medicare and Medicaid).
The report includes recommendations for policy actions that federal, state, and local policymakers and other stakeholders should take including:
- Increase funding for the CDC’s National Center for Chronic Disease Prevention and Health Programs to prevent obesity and related chronic diseases. Funding increases need to be sufficient to put proven obesity prevention programs to work in every state and should prioritize those communities where the need is greatest to address health inequities.
- Make healthy school meals for all students a permanent policy, extend COVID-19 flexibilities that expand nutrition access for students and their families, strengthen school nutrition standards, and increase students’ opportunities for physical activity during the school day.
- Expand the CDC’s social determinants of health program to address the upstream, structural drivers of chronic disease.
- Decrease food insecurity and improve the nutritional quality of available food by increasing funding for and participation in nutrition assistance programs such as the Supplemental Nutrition Assistance Program (SNAP), the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), and the Child and Adult Care Food Program.
- End unhealthy food marketing to children by closing tax loopholes and eliminating business-cost deductions related to the advertising of unhealthy food and beverages to young people.
- Impose excise taxes on sugary drinks and devote the revenue to local obesity prevention programs and to reduce health disparities.
- Expand support for maternal and child health, including supporting breastfeeding.
- Fund active transportation projects like pedestrian and biking paths in all communities and make local spaces more conducive to physical activity such as opening school recreational facilities to community groups outside of school hours.
- Expand access to healthcare and require insurance coverage with no cost sharing for U.S. Preventive Task Force recommended obesity prevention programs.
Read the full report
New Report: Nation’s Chronic Lack of Investment in Public Health Puts Americans’ Lives and Livelihoods at Risk
COVID-19 emergency funding was critical to initial pandemic response but did not address nation’s long-standing underinvestment in public health; $4.5 billion in annual infrastructure funding is needed
(Washington, DC – July 28, 2022) – Chronic underfunding has created a public health system that cannot address the nation’s health security needs, its persistent health inequities, as well as emerging threats, and, was a contributing factor in the inadequate response to the COVID-19 pandemic, according to a report, The Impact of Chronic Underfunding on America’s Public Health System: Trends, Risks, and Recommendations, 2022, released today by Trust for America’s Health.
Lack of funding in core public health programs slowed the response to the COVID-19 pandemic and exacerbated its impact, particularly in low-income communities, communities of color, and for older Americans – populations that experience higher rates of chronic disease and have fewer resources to recover from an emergency. TFAH is one of numerous organizations within the public health community calling for an annual $4.5 billion investment in public health infrastructure at the state, local, tribal, and territorial levels.
This annual report examines federal, state, and local public health funding trends and recommends investments and policy actions to build a stronger public health system, prioritize prevention, and address the ways in which social and economic inequities create barriers to good health in many communities.
“As we navigate the next stages of the pandemic and beyond, it is critical that we modernize public health data infrastructure, grow and diversify the public health workforce, invest in health promotion and prevention programs, and reduce health inequities. Investments in public health are needed in every community but should particularly be directed to those communities, which due to the impacts of structural racism, poverty, systemic discrimination, and disinvestment are placed at greatest risk during a health emergency,” said Dr. Gracia.
Emergency funding is not sufficient to address system weaknesses created by chronic underfunding
State and local public health agencies managed two divergent realities during 2021. Short-term funding was up significantly as the federal government provided funding to states and localities in an effort to control the pandemic. But this funding was one-time money and often specifically tied to COVID-19. Most of it could not be used to address longstanding deficits in the public health system, including ensuring the provision of basic public health services, replacing antiquated data systems, and growing the public health workforce. An October 2021 analysis conducted by the de Beaumont Foundation and the Public Health National Center for Innovations, found that state and local health departments need an 80 percent increase in the size of their workforce to be able to provide comprehensive public health services to their communities.
Another challenge for state and local health departments is that emergency response funding, while critical during the emergency, is too late to build prevention and preparedness programs, programs that must be in place before an emergency if they are going to protect lives. To be adequately prepared for the next public health emergency, the nation needs to sustain higher levels of public health funding and provide more flexible funding.
“Emergency funding is important but not sufficient to fill the longstanding gaps in public health investments. The ‘boom-and-bust’ cycle of public health funding has meant that the system does not have the tools or workforce to modernize and respond to the range of threats impacting our communities,” said J. Nadine Gracia, M.D., MSCE, President and CEO of Trust for America’s Health.
Funding for two key emergency preparedness and response programs are down sharply over the past two decades:
- The U.S. Centers for Disease Control and Prevention (CDC) is the country’s leading public health agency and the primary source of funding for state, local, tribal, and territorial health departments. CDC’s annual funding for Public Health Emergency Preparedness (PHEP) programs increased slightly between FY 2021 and FY 2022, from $840 million to $862 million, but has been reduced by just over one-fifth since FY 2002, or approximately in half when adjusted for inflation.
- The Hospital Preparedness Program, administered by the U.S. Department of Health and Human Services’ Office of the Assistant Secretary for Preparedness and Response, is the primary source of federal funding to help healthcare systems prepare for emergencies. It has experienced a nearly two-thirds reduction over the last two decades when adjusted for inflation.
Funding for health promotion, prevention, and equity also need sustained growth
As a nation, we spent $4.1 trillion on health in 2020 but only 5.4 percent of that spending targeted public health and prevention. Notably, this share nearly doubled last year as compared to 2019 – due to short-term COVID-19 response funding – but is still grossly inadequate and likely to return to pre-pandemic levels if the historic pattern of surging funding for public health during an emergency but neglecting it at other times resumes. Inadequate funding means that effective public health programs, such as those to prevent suicide, obesity, and environmental health threats, only reach a fraction of states. This longstanding neglect contributes to high rates of chronic disease and persistent health inequities.
Recommendations for policy actions
The report calls for policy action by the administration, Congress, and state and local officials within four areas:
Substantially increase core funding to strengthen public health infrastructure and grow the public health workforce, including increasing CDC’s base appropriation and modernizing the nation’s public health data and disease tracking systems.
Invest in the nation’s health security by increasing funding for public health emergency preparedness, including within the healthcare system, improving immunization infrastructure, and addressing the impacts of climate change.
Address health inequities and their impact on root causes of disease by addressing the social determinants of health that have an outsized impact on health outcomes.
Safeguard and improve health across the lifespan. Many programs that promote health and prevent the leading causes of disease, disability, and death have been long neglected and do not reach all states or the populations most at risk. Reinvigorating programs that stem chronic disease, support children and families, and prevent substance misuse and suicide should be a top priority.
Read the full report
The Impact of Chronic Underfunding on America’s Public Health System: Trends, Risks, and Recommendations, 2022
Over Thirty-Five Health and Child Wellness Organizations Endorse the Improving Data Collection for Adverse Childhood Experiences Act
(Washington, DC – July 11, 2022) – Adverse Childhood Experiences (ACEs) can have long-lasting effects over the lifetime of an individual including negative health impacts. Research shows that the higher the number of ACEs an individual experiences the higher their risk for negative health outcomes like asthma, diabetes, cancer, substance use, and suicide in adulthood. The Centers for Disease Control and Prevention estimate that 61 percent of U.S. adults report having at least one ACE, and that the prevention of ACEs could reduce cases of depression in adults by 44 percent and avoid 1.9 million cases of heart disease.
The Improving Data Collection for ACEs Act is a bipartisan effort to enable the collection of more inclusive data about ACEs. It would support additional research on the impact of ACEs with a focus on understanding of the frequency and intensity of ACEs, the relationship between ACEs and negative health outcomes, and the influence of risk and protective factors.
For more information, contact Brandon Reavis, Senior Government Relations Manager at Trust for America’s Health, [email protected].