A medida que aumentan las amenazas, la evaluación anual determina que el nivel de preparación de los estados para emergencias sanitarias está mejorando en algunas áreas, pero está estancado en otras
(Washington, DC) – Veinticinco Estados y el Distrito de Columbia tuvieron un alto desempeño en una medida de tres niveles de preparación de los Estados para proteger la salud public durante una emergencia, según un nuevo informe publicado hoy por Trust for America’s Health (TFAH, por su sigla en inglés). El informe anual, Ready or Not 2020: Proteging the Public’s Health from Diseases, Disasters and Bioterrorism, encontró una mejora año tras año entre las 10 medidas de preparación para emergencias, pero también señala áreas que necesitan mejoras. El año pasado, 17 Estados se clasificaron en el nivel superior del informe.
Para 2020, 12 Estados se ubicaron en el nivel de rendimiento medio, por debajo de 20 Estados y el Distrito de Columbia en el nivel medio el año pasado, y 13 se ubicaron en el nivel de rendimiento bajo, el mismo número que el año pasado.
El informe encontró que el nivel de preparación de los estados ha mejorado en áreas claves, que incluyen fondos de salud pública, participación en coaliciones y pactos de atención médica, seguridad hospitalaria y vacunación contra la gripe. Sin embargo, otras medidas clave de seguridad de la salud, que incluyen garantizar un suministro de agua seguro y acceso a tiempo libre remunerado, está estancado o perdido.
| Nivel de Rendimiento | Estados | Numero de Estados |
| Alto | AL, CO, CT, DC, DE, IA, ID, IL, KS, MA, MD, ME, MO, MS, NC, NE, NJ, NM, OK, PA, TN, UT, VA, VT, WA, W |
25 Estados y DC |
| Medio | AZ, CA, FL, GA, KY, LA, MI, MN, ND, OR, RI, TX | 12 Estados |
Bajo |
AK, AR, HI, IN, MT, NH, NV, NY, OH, SC, SD, WV, WY | 13 Estados |
El informe mide el desempeño anualmente de los Estados utilizando 10 indicadores que, en conjunto, proporcionan una lista de verificación del nivel de preparación de una jurisdicción para prevenir y responder a las amenazas a la salud de sus residentes durante una emergencia. Los indicadores son:
| Indicadores de Preparación | |||
| 1 | Gestión de incidentes: adopción del Pacto de licencia de enfermería | 6 | Seguridad del agua: Porcentaje de la población que utilizó un sistema de agua comunitario que no cumplió con todos los estándares de salud aplicables. |
| 2 | Colaboración comunitaria intersectorial: porcentaje de hospitales que participan en coaliciones de atención médica. | 7 | Resistencia laboral y control de infecciones: porcentaje de población ocupada con tiempo libre remunerado. |
| 3 | Calidad institucional: acreditación de la Junta de Acreditación de Salud Pública | 8 | Utilización de contramedidas: porcentaje de personas de 6 meses o más que recibieron una vacuna contra la gripe estacional. |
| 4 | Calidad institucional: acreditación del Programa de acreditación de gestión de emergencias. | 9 | Seguridad del paciente: porcentaje de hospitales con una clasificación de alta calidad (grado “A”) en el grado de seguridad del hospital Leapfrog. |
| 5 | Calidad institucional: tamaño del presupuesto estatal de salud pública, en comparación con el año pasado. | 10 | Vigilancia de la seguridad de la salud: el laboratorio de salud pública tiene un plan para un aumento de la capacidad de prueba de seis a ocho semanas. |
Cuatro Estados (Delaware, Pensilvania, Tennessee y Utah) pasaron del nivel de bajo rendimiento en el informe del año pasado al nivel alto en el informe de este año. Seis Estados (Illinois, Iowa, Maine, Nuevo México, Oklahoma, Vermont) y el Distrito de Columbia pasaron del nivel medio al nivel alto. Ningún Estado cayó del nivel alto al bajo, pero seis pasaron del nivel medio al bajo: Hawaii, Montana, Nevada, New Hampshire, Carolina del Sur y Virginia Occidental.
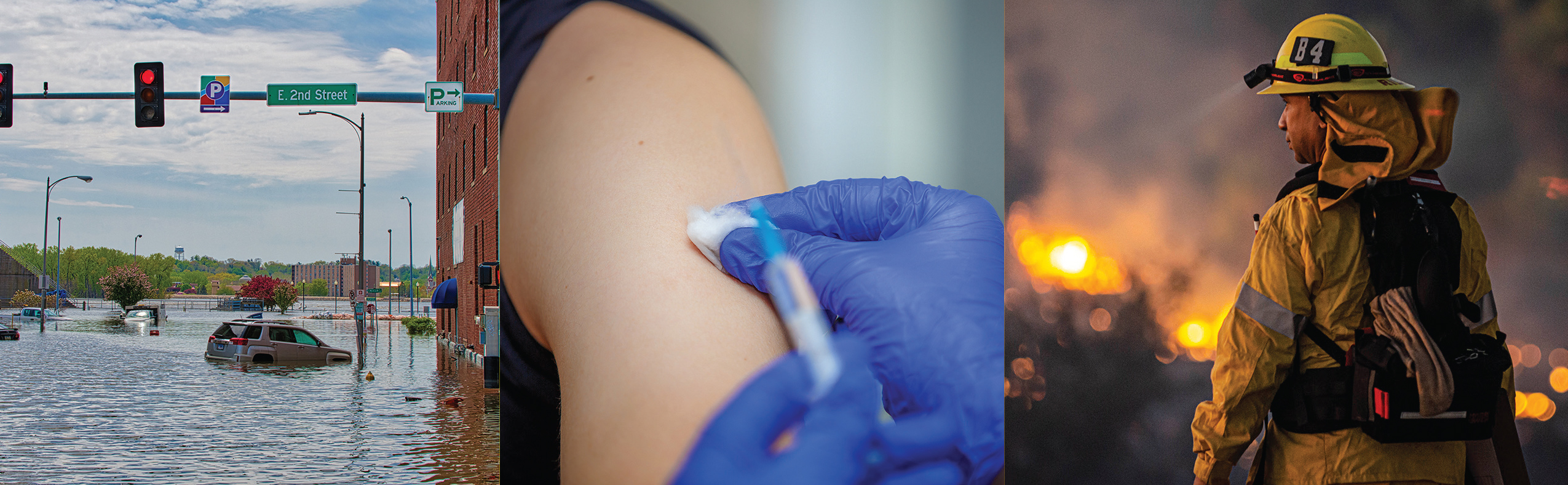
“El creciente número de amenazas para la salud de los estadounidenses en 2019, desde inundaciones hasta incendios forestales y vapeo, demuestra la importancia crítica de un sistema de salud pública sólido. Estar preparado es a menudo la diferencia entre daños o no daños durante emergencias de salud y requiere cuatro cosas: planificación, financiamiento dedicado, cooperación interinstitucional y jurisdiccional, y una fuerza laboral calificada de salud pública “, dijo John Auerbach, presidente y CEO de Trust for America’s Health.
“Si bien el informe de este año muestra que, como nación, estamos más preparados para enfrentar emergencias de salud pública, todavía no estamos tan preparados como deberíamos estar”. Se necesita más planificación e inversión para salvar vidas”, dijo Auerbach.
El análisis de TFAH encontró que:
- La mayoría de los Estados tienen planes para expandir la capacidad de atención médica en una emergencia a través de programas como el Pacto de Licencias de Enfermería u otras coaliciones de atención médica. Treinta y dos Estados participaron en el Pacto de Licencias de Enfermeras, que permite a las enfermeras licenciadas practicar en múltiples jurisdicciones durante una emergencia. Además, el 89 por ciento de los hospitales a nivel nacional participaron en una coalición de atención médica, y 17 estados y el Distrito de Columbia tienen participación universal, lo que significa que todos los hospitales del estado (+ DC) participaron en una coalición. Además, 48 Estados y DC tenían un plan para aumentar la capacidad del laboratorio de salud pública durante una emergencia.
- La mayoría de los Estados están acreditados en las áreas de salud pública, manejo de emergencias o ambos. Dicha acreditación ayuda a garantizar que los sistemas necesarios de prevención y respuesta ante emergencias estén implementados y que cuenten con personal calificado.
- La mayoría de las personas que tienen agua de su hogar a través de un sistema de agua comunitario tenían acceso a agua segura. Según los datos de 2018, en promedio, solo el 7 por ciento de los residentes estatales obtuvieron el agua de su hogar de un sistema de agua comunitario que no cumplía con los estándares de salud aplicables, un poco más del 6 por ciento en 2017.
- Las tasas de vacunación contra la gripe estacional mejoraron, pero aún son demasiado bajas. La tasa de vacunación contra la gripe estacional entre los estadounidenses de 6 meses en adelante aumentó del 42 por ciento durante la temporada de gripe 2017-2018 al 49 por ciento durante la temporada 2018-2019, pero las tasas de vacunación todavía están muy por debajo del objetivo del 70 por ciento establecido por Healthy People 2020.
- En 2019, solo el 55 por ciento de las personas empleadas tenían acceso a tiempo libre remunerado, el mismo porcentaje que en 2018. Se ha demostrado que la ausencia de tiempo libre remunerado exacerba algunos brotes de enfermedades infecciosas. También puede evitar que las personas reciban atención preventiva.
- Solo el 30 por ciento de los hospitales, en promedio, obtuvieron las mejores calificaciones de seguridad del paciente, un poco más que el 28 por ciento en 2018. Los puntajes de seguridad hospitalaria miden el desempeño en temas tales como las tasas de infección asociadas a la atención médica, la capacidad de cuidados intensivos y una cultura general de prevención de errores. Dichas medidas son críticas para la seguridad del paciente durante los brotes de enfermedades infecciosas y también son una medida de la capacidad del hospital para funcionar bien durante una emergencia.
Otras secciones del informe describen cómo el sistema de salud pública fue fundamental para la respuesta a la crisis de vapeo, cómo las inequidades en salud ponen a algunas comunidades en mayor riesgo durante una emergencia y las necesidades de las personas con discapacidad durante una emergencia.
Se puede acceder al informe completo en Ready or Not 2020 report. |
# # #
Trust for America’s Health es una organización sin fines de lucro y no partidista que promueve la salud óptima para cada persona y comunidad y hace de la prevención de enfermedades y lesiones una prioridad nacional. www.tfah.org. Twitter: @ healthyamerica1