Since its launch in July 2022, the 988 Suicide and Crisis Lifeline has responded to millions of individuals and has provided immediate support to callers who are in crisis. Still, recent and proposed cuts to the Substance Abuse and Mental Health Services Administration (SAMHSA) and 988 services and the lack of state funding could leave individuals in need or others with fewer options for life-saving help.
The national 988 Suicide and Crisis Lifeline has answered more than 14 million calls, texts, and chats since it was introduced. Call volume to the Lifeline in the first two years of its existence was up 95 percent nationally as compared to calls to the 1-800 system it replaced. In addition, call answer rates have improved and wait times have been reduced.
Still, recent major cuts to agency workforce and a recent decision to end specialized services through 988 for LGBTQIA+ youth and young adults is poised to set that progress back and could have dire consequences.
Brief History
The 988 Suicide and Crisis Lifeline was established by Congress in 2020 and launched officially in 2022 in an effort to enhance the nation’s crisis care system. Established by Congress, 988 was designed to make the previous seven-digit 1-800 suicide prevention lifeline more accessible by creating an easy to remember call number and adding a text option. In 2024, calls and texts began being routed to local crisis centers based on geographic location instead of area codes to help connect users with faster and local support.
In addition, the 988 Lifeline has included specialized support for military veterans, LGTBQIA+ youth, and Spanish-language speakers. To address the disproportionate rates of suicide among American Indian and Alaska Native populations and provide culturally and trauma informed crisis services, the state of Washington offers specialized care for Washington’s American Indian and Alaska Native communities.
People seeking assistance through the 988 Lifeline are able to call, text, and chat through the website with trained professionals at 988 call centers. Counselors either counsel callers through their crisis or direct individuals to acute care in their community.
Research from the American Association of Suicidology found that two-thirds of the people who had suicidal thoughts and reached out via the Lifeline’s online chat reported that the correspondence had been helpful, and 45% reported being less suicidal.
The Need and Demand for the Crisis Lifeline
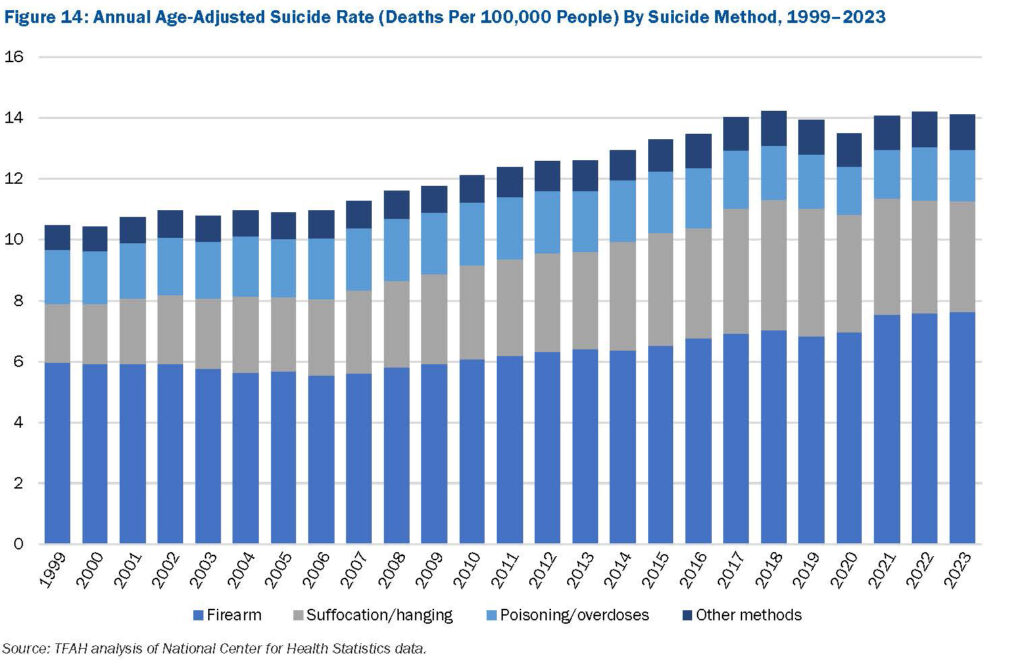
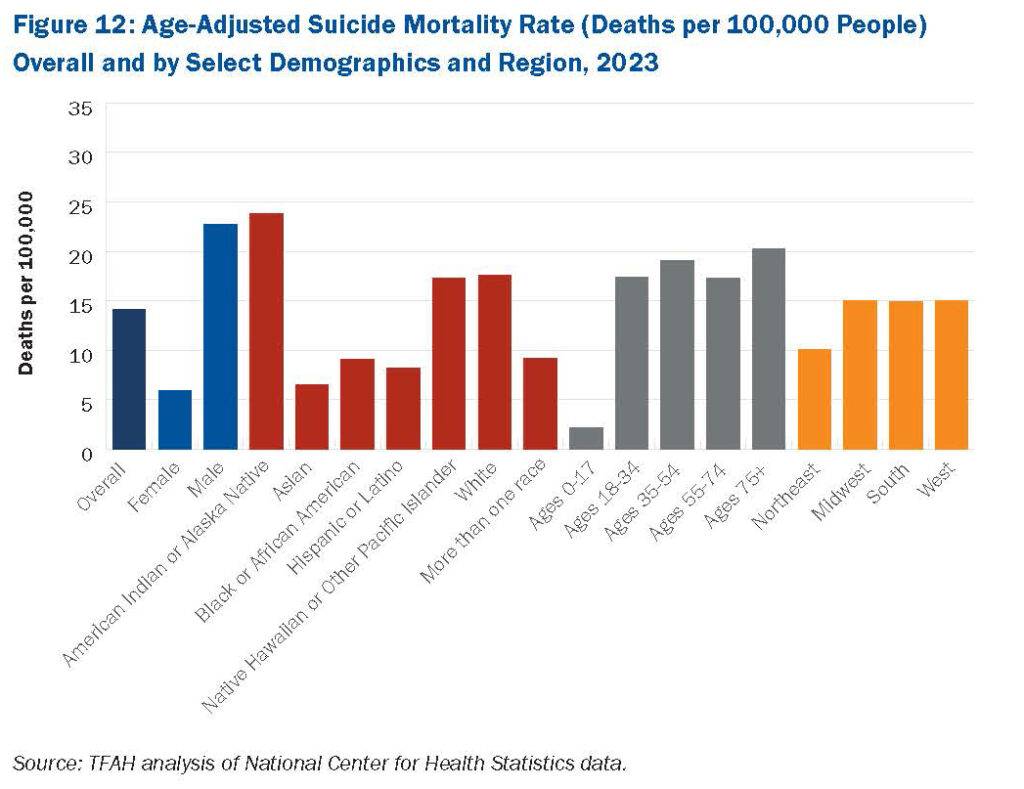 According to the latest edition of Trust for America’s Health’s Pain in the Nation: The Epidemics of Alcohol, Drug, and Suicide Deaths report, nearly 50,000 Americans of all ages died by suicide in 2023. Although there has been some fluctuation over the past few years, suicide rates have generally been on the rise since 1999. Nearly a half million people died from died by suicide in the U.S. from 2014 to 2023.
According to the latest edition of Trust for America’s Health’s Pain in the Nation: The Epidemics of Alcohol, Drug, and Suicide Deaths report, nearly 50,000 Americans of all ages died by suicide in 2023. Although there has been some fluctuation over the past few years, suicide rates have generally been on the rise since 1999. Nearly a half million people died from died by suicide in the U.S. from 2014 to 2023.
 Some of the highest age-adjusted suicide rates are seen in males and adults ages 75 and older. Suicide rates in rural areas are consistently and significantly higher than urban areas, research shows as well.
Some of the highest age-adjusted suicide rates are seen in males and adults ages 75 and older. Suicide rates in rural areas are consistently and significantly higher than urban areas, research shows as well.
To turn the tide, TFAH urges federal and state policymakers to transform the nation’s mental health and substance use prevention system, in part by strengthening the continuum of crisis intervention supports and programs. TFAH also urges federal agencies to do more to encourage and make people feel more comfortable seeking help with mental health issues, for example by promoting culturally appropriate messaging on mental health screening and treatment to reduce stigma. The 988 Lifeline provides a pathway for states and local communities to implement those recommendations.
Federal and State Support Needs to be Sustained and Increased
The 988 Lifeline is funded primarily through federal funding and is administered by the Substance Abuse and Mental Health Services Administration (SAMHSA). Some states provide additional funding support through their annual budgets and/or telecommunications fees. To date, 16 states are providing funding for their 988 networks. Unfortunately, there are ongoing threats to funding for 988 and suicide prevention services. In March 2025, the Department of Health and Human Services (HHS) announced they would be clawing back $1 billion in SAMHSA funds, including mental health grants many states were applying to 988 suicide lifelines and crisis services. Litigation is putting this clawback on hold in some states. In addition, reductions in force at SAMHSA and the President’s FY 26 Budget Request which proposes to eliminate SAMHSA and significantly reduce mental health programs and funding, could undo progress communities are making in addressing suicide, mental health, and substance use crises.
Where Do We Go From Here?
To continue to support the nation’s crisis services, the following action steps are needed:
- Congress and the Administration should strengthen the 988 Suicide and Crisis Lifeline by maintaining SAMHSA funding for the Lifeline and by restoring the workforce devoted to these services. SAMHSA should also retain the 988 Lifeline’s specialized services, including specialized support for LGBTQIA+ youth and Spanish-language services.
- Congress should also pass the 9-8-8 Implementation Act, which would authorize funding for crisis call centers to purchase or upgrade call center technology, hire and train call center staff, and improve call center operations.
- More states should dedicate funding for the 988 Lifeline and more investments should be made to improve geo-location technology so people that need help are directed to services in their community.


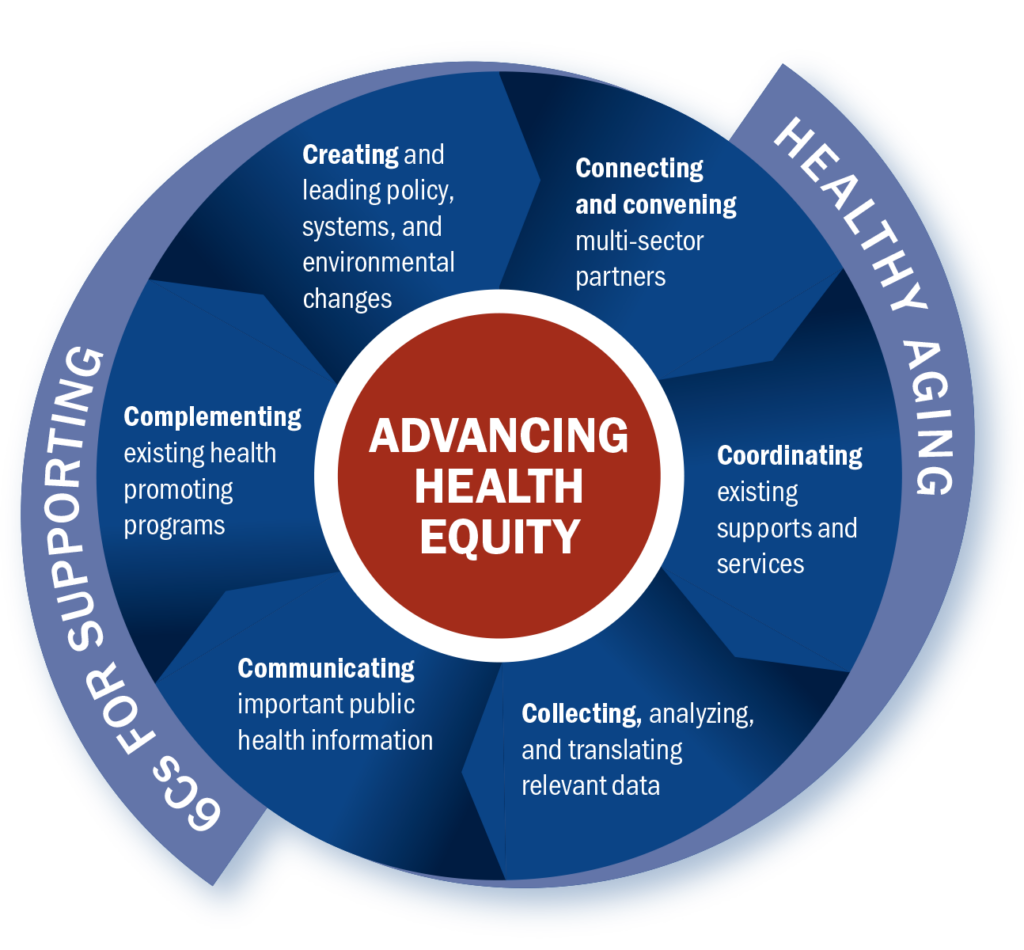 Megan: The Guide can be used by anyone who wants to build expertise in healthy aging, especially from a public health perspective. Our vision is that entire health department staffs will use it, but it’s also perfect for individuals or small teams to work through together.
Megan: The Guide can be used by anyone who wants to build expertise in healthy aging, especially from a public health perspective. Our vision is that entire health department staffs will use it, but it’s also perfect for individuals or small teams to work through together.