As Threats Increase, Annual Assessment Finds States’ Level of Readiness for Health Emergencies is Improving in Some Areas but Stalled in Others
February 5, 2020
(Washington, DC) – Twenty-five states and the District of Columbia were high-performers on a three-tier measure of states’ preparedness to protect the public’s health during an emergency, according to a new report released today by Trust for America’s Health (TFAH). The annual report, Ready or Not 2020: Protecting the Public’s Health from Diseases, Disasters, and Bioterrorism, found year-over-year improvement among 10 emergency readiness measures, but also notes areas in need of improvement. Last year, 17 states ranked in the report’s top tier.
For 2020, 12 states placed in the middle performance tier, down from 20 states and the District of Columbia in the middle tier last year, and 13 placed in the low performance tier, the same number as last year.
The report found that states’ level of preparedness has improved in key areas, including public health funding, participation in healthcare coalitions and compacts, hospital safety, and seasonal flu vaccination. However, other key health security measures, including ensuring a safe water supply and access to paid time off, stalled or lost ground.
| Performance Tier | States | Number of States |
| High Tier | AL, CO, CT, DC, DE, IA, ID, IL, KS, MA, MD, ME, MO, MS, NC, NE, NJ, NM, OK, PA, TN, UT, VA, VT, WA, WI |
25 states and DC |
| Middle Tier | AZ, CA, FL, GA, KY, LA, MI, MN, ND, OR, RI, TX | 12 states |
| Low Tier | AK, AR, HI, IN, MT, NH, NV, NY, OH, SC, SD, WV, WY | 13 states |
The report measures states’ performance on an annual basis using 10 indicators that, taken together, provide a checklist of a jurisdiction’s level of preparedness to prevent and respond to threats to its residents’ health during an emergency. The indicators are:
| Preparedness Indicators | |||
| 1 | Incident Management: Adoption of the Nurse Licensure Compact. | 6 | Water Security: Percentage of the population who used a community water system that failed to meet all applicable health-based standards. |
| 2 | Cross-Sector Community collaboration: Percentage of hospitals participating in healthcare coalitions. | 7 | Workforce Resiliency and Infection Control: Percentage of employed population with paid time off. |
| 3 | Institutional Quality: Accreditation by the Public Health Accreditation Board. | 8 | Countermeasure Utilization: Percentage of people ages 6 months or older who received a seasonal flu vaccination. |
| 4 | Institutional Quality: Accreditation by the Emergency Management Accreditation Program. | 9 | Patient Safety: Percentage of hospitals with a top-quality ranking (“A” grade) on the Leapfrog Hospital Safety Grade. |
| 5 | Institutional Quality: Size of the state public health budget, compared with the past year. | 10 | Health Security Surveillance: The public health laboratory has a plan for a six-to eight-week surge in testing capacity. |
Four states (Delaware, Pennsylvania, Tennessee, and Utah) moved from the low performance tier in last year’s report to the high tier in this year’s report. Six states (Illinois, Iowa, Maine, New Mexico, Oklahoma, Vermont) and the District of Columbia moved up from the middle tier to the high tier. No state fell from the high to the low tier but six moved from the middle to the low tier. Hawaii, Montana, Nevada, New Hampshire, South Carolina, and West Virginia.
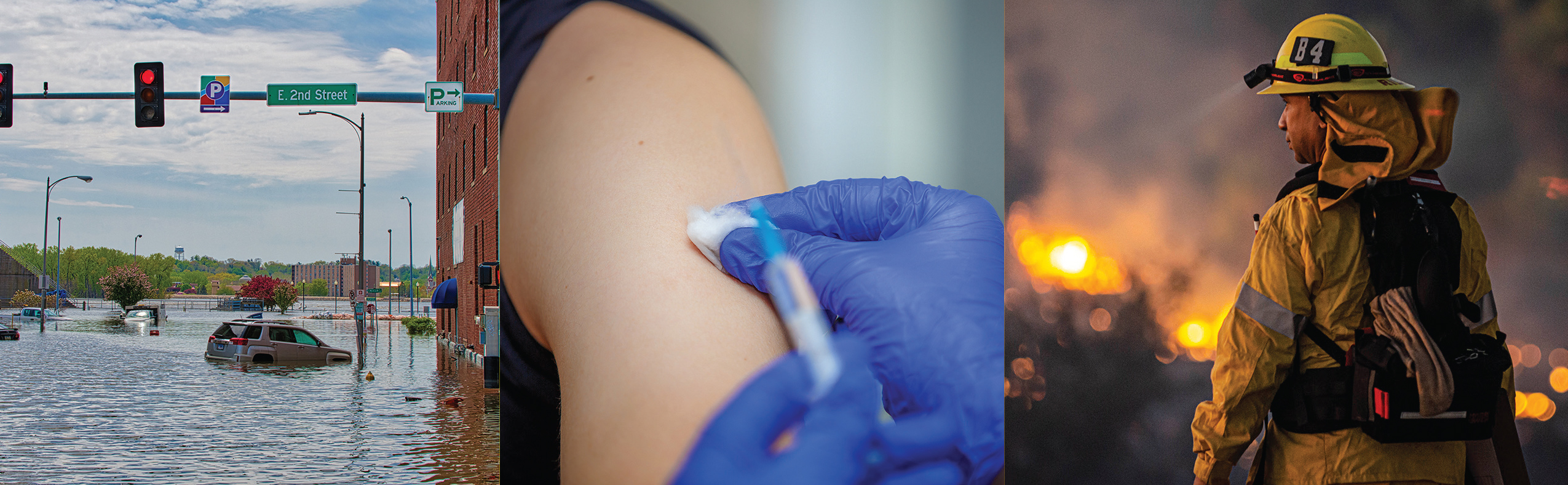
“The increasing number of threats to Americans’ health in 2019, from floods to wildfires to vaping, demonstrate the critical importance of a robust public health system. Being prepared is often the difference between harm or no harm during health emergencies and requires four things: planning, dedicated funding, interagency and jurisdictional cooperation, and a skilled public health workforce,” said John Auerbach, President and CEO of Trust for America’s Health.
“While this year’s report shows that, as a nation, we are more prepared to deal with public health emergencies, we’re still not as prepared as we should be. More planning and investment are necessary to saves lives,” Auerbach said.
TFAH’s analysis found that:
- A majority of states have plans in place to expand healthcare capacity in an emergency through programs such as the Nurse Licensure Compact or other healthcare coalitions. Thirty-two states participated in the Nurse Licensure Compact, which allows licensed nurses to practice in multiple jurisdictions during an emergency. Furthermore, 89 percent of hospitals nationally participated in a healthcare coalition, and 17 states and the District of Columbia have universal participation meaning every hospital in the state (+DC) participated in a coalition. In addition, 48 states and DC had a plan to surge public health laboratory capacity during an emergency.
- Most states are accredited in the areas of public health, emergency management, or both. Such accreditation helps ensure that necessary emergency prevention and response systems are in place and staffed by qualified personnel.
- Most people who got their household water through a community water system had access to safe water. Based on 2018 data, on average, just 7 percent of state residents got their household water from a community water system that did not meet applicable health standards, up slightly from 6 percent in 2017.
- Seasonal flu vaccination rates improved but are still too low. The seasonal flu vaccination rate among Americans ages 6 months and older rose from 42 percent during the 2017-2018 flu season to 49 percent during the 2018-2019 season, but vaccination rates are still well below the 70 percent target established by Healthy People 2020.
- In 2019, only 55 percent of employed people had access to paid time off, the same percentage as in 2018. The absence of paid time off has been shown to exacerbate some infectious disease outbreaks . It can also prevent people from getting preventive care.
- Only 30 percent of hospitals, on average, earned top patient safety grades, up slightly from 28 percent in 2018. Hospital safety scores measure performance on such issues as healthcare associated infection rates, intensive-care capacity and an overall culture of error prevention. Such measures are critical to patient safety during infectious disease outbreaks and are also a measure of a hospital’s ability to perform well during an emergency.
The report includes recommended policy actions that the federal government, states and the healthcare sector should take to improve the nation’s ability to protect the public’s health during emergencies.
Other sections of the report describe how the public health system was critical to the vaping crisis response, how health inequities put some communities at greater risk during an emergency, and the needs of people with disabilities during an emergency.
Read the full text report |