State of Obesity 2024: Better Policies for a Healthier America
This report tracks U.S. obesity rates by state, race, gender, and age and offers policy solutions. Obesity rates nationwide continue to be at epidemic levels and are predominantly highest in communities experiencing barriers to healthy eating and those with few opportunities for physical activity.
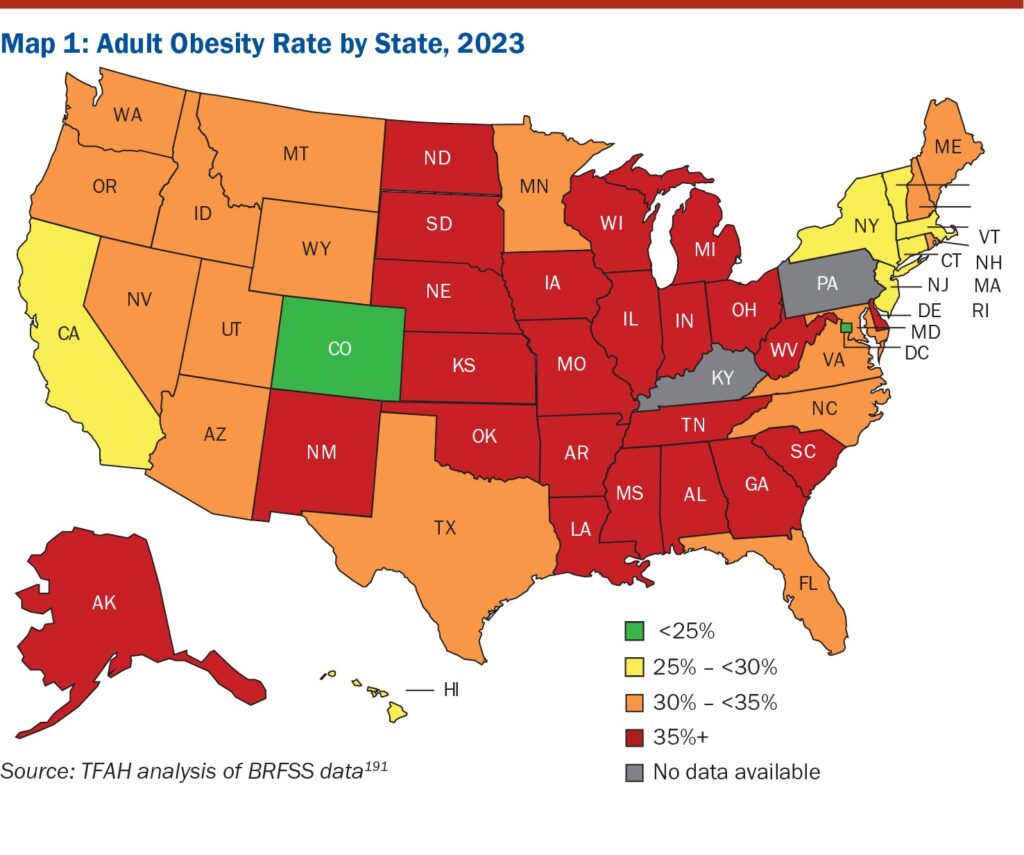
(Washington, DC – September 12, 2024) – Obesity rates for U.S. adults were at or higher than 35 percent in twenty-three states in 2023, part of a multi-decade increase in the rates of Americans living with obesity. In comparison, in 2012, no state had an adult obesity rate at or above 35 percent.
The report, State of Obesity 2024: Better Policies for a Healthier America includes TFAH’s analysis of the latest data from the Centers for Disease Control and Prevention’s (CDC) Behavioral Risk Factor Surveillance System. Obesity and other diet-related diseases are associated with a range of physical and mental health conditions, higher mortality, higher healthcare costs, and productivity losses.
The states with the highest rates of obesity among adults in 2023 were West Virginia (41.2 percent), Mississippi (40.1 percent), Arkansas (40.0 percent), Louisiana (39.9 percent), and Alabama (39.2 percent). Between 2022 and 2023, three states experienced statistically significant increases in their adult obesity rates: Alaska, Arkansas, and Oregon, while no states had a statistically significant decline. Between 2018 and 2023, 28 states have experienced statistically significant increases in adult obesity rates.
States with lowest levels of adult obesity in 2023 were Colorado (24.9 percent), Hawaii (26.1 percent), Massachusetts (27.4 percent), and California (27.7 percent), plus the adult obesity rate in the District of Columbia was 23.5 percent.
Nationally, over four in 10 U.S. adults have obesity. While obesity rates have increased for all population groups, groups with the highest rates, often populations of color, typically face structural barriers to healthy eating, including food cost and access, and a lack of opportunities and places to be physically active. Black and Latino adults and people living in rural communities tend to have the highest rates of obesity.
Obesity rates are also increasing among children and adolescents, with nearly 20 percent of U.S. children and adolescents, ages 2 to 19, having obesity. These rates have more than tripled since the mid-1970s, and Black and Latino youth have substantially higher rates of obesity compared to their white peers.
The impact of the food environment on obesity rates
A special section within the report looks at the country’s food environment and factors that affect food consumption such as food policy, supply, access, and pricing, and the influence of food advertising on what people eat. The section discusses opportunities for policymakers to make the food environment more conducive to healthy eating, especially within low-income communities.
“As the number of people living with obesity, as well as the rates of obesity-related disease continue to rise, there’s an urgent need for systems level policy responses,” said J. Nadine Gracia, M.D., MSCE, President and CEO of Trust for America’s Health. “The obesity epidemic is not only about individual behavior; socioeconomic and environmental factors which are largely beyond any one person’s control have a significant role. Policymakers need to act to address this growing health crisis.”
Policy action is needed
The report includes evidence-based policy recommendations for federal, state, and local officials, as well as other stakeholders such as the healthcare sector and the food industry. Recommended policy actions include:
Increase federal resources for effective efforts that reduce obesity-related disparities and related conditions including funding for CDC’s chronic disease and obesity prevention programs, including State Physical Activity and Nutrition, Racial and Ethnic Approaches to Community Health, and Healthy Tribes programs.
Decrease food and nutrition insecurity while improving the nutritional quality of available foods in every community by, among other activities, providing healthy school meals for all students and maintaining progress on the final 2024 school nutritional meal standards. In addition, Congress should expand access to nutrition support programs such as the Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) and increase the value of their benefits.
To help consumers make informed choices, the Food and Drug Administration should swiftly implement a front-of-package label that will help people more easily understand the nutrients in packaged foods.
Eliminate tax loopholes and business cost deductions for the advertising of unhealthy foods and beverages to children. Healthy food and drink choices can also be encouraged by taxing sugar-sweetened beverages.
Ensure that every community has a built environment that encourages active transportation, e.g., walking and biking to everyday destinations, and safe places to be physically active including parks and other places for indoor and outside play.
Policymakers, healthcare, public health, and other stakeholders should close gaps in healthcare access by expanding Medicaid and by making marketplace coverage more affordable. Medicaid, Medicare, and other payers should cover obesity-related services without patient cost sharing.
Congress should address root causes of chronic diseases by incentivizing multi-sector collaborations to address social and nonmedical drivers of health and healthcare and insurers should continue to expand strategies to screen and reimburse for patients’ health-related social needs.

