Local health officials and CDC work together to stamp out Ohio measles outbreak
In 1912, the United States formally recognized measles—a highly contagious viral infection causing fever, cough, runny nose, red eyes, and a characteristic rash in milder cases, while leading to pneumonia, encephalitis, and death in more severe instances—as a nationally notifiable disease. For centuries, this ubiquitous childhood ailment afflicted millions. In the first decade of reporting, an annual average of 6,000 measles-related fatalities were recorded in the U.S.
The introduction of the first measles vaccine in 1963, with its near-perfect efficacy, marked a turning point. The vaccine was later combined with those for mumps and rubella (MMR) in 1971, and varicella (MMRV) in 2005, providing children protection against several diseases in a single shot. Bolstered by this potent new preventive tool, the Centers for Disease Control and Prevention (CDC) set a goal in 1978 to eliminate measles from the country. This objective was realized in 2000, thanks to robust vaccination campaigns, the introduction of a second dose in 1989 to increase efficacy, and rigorous disease surveillance systems.
In the new millennium, measles appeared a relic of the past, but the specter of outbreaks returned—first in the 2014-15 Disneyland episode, and then in the largest outbreak in decades in 2019. Declining vaccination rates, fueled by skepticism and misinformation, left vulnerable communities exposed. The 2019 outbreak primarily affected unvaccinated children in communities with low vaccination rates across 31 states, such as ultra-Orthodox Jewish communities in New York and vaccine hesitant regions in Washington. Travelers imported the virus, sparking infections among the unvaccinated.
One such measles outbreak erupted in Ohio in 2022. Between November 2022 and February 2023, when the outbreak was declared over, 85 cases were reported, primarily affecting children under five, with 36 hospitalizations. Among the 85 cases, 80 were unvaccinated, including 25 infants too young to receive their first dose.
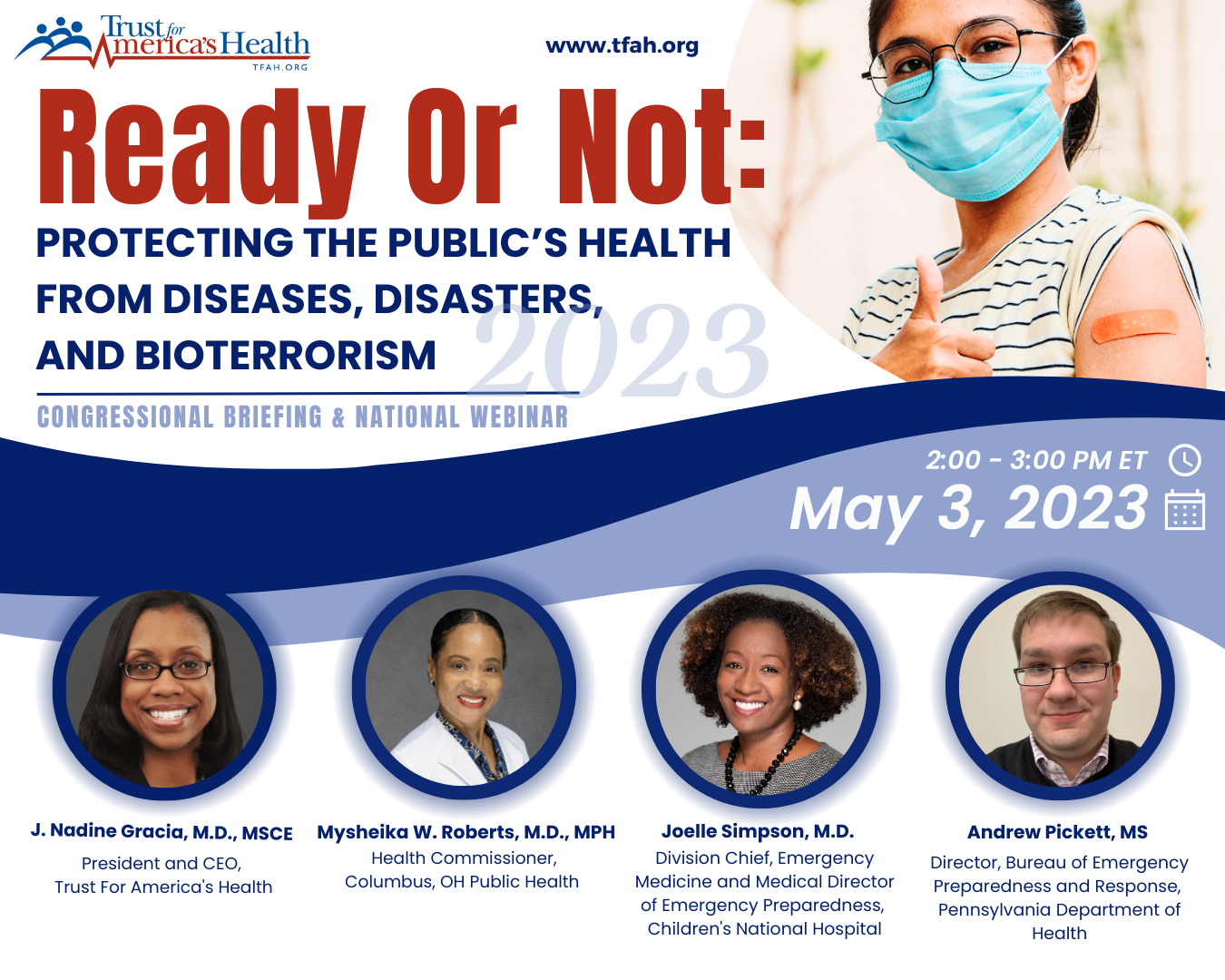
To quell the outbreak, a team of epidemiologists from the CDC worked in concert with Columbus Public Health to track cases, identify and notify exposed residents, and understand the spread of the virus. Dr. Mysheika Roberts, Columbus’s health commissioner, led the outbreak response, raising awareness of the disease through public information and education, and promoting and easing access to vaccination.
In addition to the on-the-ground work of state and local health departments, the CDC plays a vital, often behind-the-scenes role in supporting those departments and safeguarding public health. It provides robust disease surveillance systems, expert guidance, technical assistance, and financial support, enabling locally targeted interventions and infrastructure improvements.
Though the latest outbreak was successfully contained, the Ohio measles episode may portend further challenges. Vaccine hesitancy, a complex and deeply ingrained phenomenon, threatens to erode hard-won public health gains and could precipitate resurgent outbreaks. The issue has multifaceted roots including mistrust in science and institutions, and misinformation amplified on digital platforms. In communities of color, vaccine hesitancy is compounded by longstanding health disparities and medical mistreatment.
The COVID-19 pandemic exacerbated the problem, with routine vaccination rates falling due to school closures and disrupted well-child doctor visits. A recent Kaiser Family Foundation poll revealed that, amid the politicization of COVID-19 vaccines and school mandates, over a third of parents with children under 18 believe they should have the choice to not vaccinate their children against measles, mumps, and rubella, even at the risk of others’ health. This represents a 52% increase compared to 2019. During the 2021-22 school year, kindergarten vaccination coverage fell to roughly 93%, leaving about 250,000 kindergartners potentially unprotected against measles.
Tackling vaccine hesitancy and strengthening our public health systems requires a multifaceted national approach. Federal, state, and local governments should invest in accessible, science-based education campaigns that dispel myths and foster trust. Working with local partners, public health agencies are developing tailored, culturally sensitive vaccine education and access programs that bridge gaps in understanding and acceptance.
The Ohio measles outbreak serves as a stark reminder that the fight against vaccine-preventable diseases remains ongoing, the indispensable role of the public health workforce, and the critical need for a robust public health system. Increased, sustained, and flexible public health funding is key to having such a system. As is growing a diverse workforce to ensure that those shaping policy and delivering services reflect the communities they serve. By taking these steps, among others, we can reduce vaccine hesitancy, create a more robust public health system, and foster an environment of trust in science. Doing so can protect the hard-won progress made against measles and other diseases, safeguard the health and well-being of generations to come, and pave the way for a more equitable future.