Issue Category: Child and School Health
COVID-19 School Closures Put 30 Million Children at Risk of Hunger
Many States with High COVID-19 Infection Rates Also Have Highest School-Meal Programs Participation Rates
(Washington, DC – July 16, 2020) – As COVID-19 infection rates continue to increase in states across the country, many of those jurisdictions are facing the complex dilemma of high infections rates complicating school re-openings and thereby limiting students’ access to school-based meal programs. Among the states with spiking infection rates and a high percentage of students participating in school-based meal programs are Arizona, Florida, Louisiana, Mississippi and South Carolina.
In March schools across the country began closing to stop the spread of the COVID-19 virus. In response, and recognizing the important source of nutrition school-based meals were to millions of American children, the U.S. Department of Agriculture’s Food and Nutrition Service began approving nationwide waivers to provide school systems flexibility in how meals were provided to students. For example, these waivers enable schools to serve meals in non-congregate settings and outside of standard mealtimes, serve afterschool snacks and meals outside of structured environments, and waive requirements that students be present when meals are picked up.
Over half of all students in elementary and secondary schools across the country depend on the National School Lunch Program, and 12.5 million of those students also participate in the School Breakfast Program. As the COVID-19 pandemic closed schools this spring, these students were placed at risk of not having enough to eat.
A new policy brief, Beyond School Walls: How Federal, State and Local Entities are Adapting Policies to Ensure Student Access to Healthy Meals During the COVID-19 Pandemic, released today by Trust for America’s Health, reviews steps the federal and state governments have taken to ensure students’ access to healthy meals when schools are closed and what needs to be done to ensure continued meal access as all school systems face uncertainties about how to safely reopen for the 2020-2021 school year.
“School meal programs are the most important source of nutritious food for millions of American children. To the degree possible, school systems, with financial and regulatory relief from the federal government, should continue to be innovative about how to deliver meals to students and should strive to meet or exceed federal nutrition standards for these meals despite product shortages created by the pandemic,” said Adam Lustig, Project Manager at Trust for America’s Health and the brief’s author.
Due to the economic impact the pandemic has had on millions of American families and the numerous uncertainties about how to safely re-open schools, the currently in place program waivers should be extended through the summer and may need to be kept in place during the 2020–2021 school year, the brief says.
Many of the states hardest hit by COVID also have highest school meal programs participation rates
States with some of the highest rates of COVID-19 infections also have high percentages of students who depend on school meals for much of their nutrition. States in which both COVID-19 infection rates are above national medians and school meals program enrollment is high include Arizona, Florida, Georgia, Louisiana, Mississippi, and South Carolina.
States in which more than half of students are enrolled in school-meals programs are:
Percentage of students enrolled in school meal programs
D.C. 76.4%
Mississippi 75.0%
New Mexico 71.4%
South Carolina 67.0%
Arkansas 63.6%
Louisiana 63.0%
Oklahoma 62.5%
Georgia 62.0%
Nevada 60.8%
Kentucky 58.7%
California 58.1%
Florida 58.1%
Arizona 57.0%
Missouri 52.7%
New York 52.6%
Illinois 50.2%
Alabama 51.6%
Oregon 50.5%
Hunger, poor nutrition and food insecurity can increase a child’s risk of developing a range of physical, mental, behavioral, emotional, and learning problems. Hungry children also get sick more often and are more likely to be hospitalized. Maintaining children’s access to nutritious meals despite school closures not only ensure they do not go hungry, but also promotes children’s health.
“State and federal guidelines waivers have allowed school systems to provide meals to students during the pandemic response, keeping them in place this summer and into the 2020-2021 school year will be the difference between kids who have enough to eat and kids who go hungry,” Lustig said.
# # #
Trust for America’s Health is a nonprofit, nonpartisan organization that promotes optimal health for every person and community and makes the prevention of illness and injury a national priority. Twitter:@HealthyAmerica1
Newly Announced Order for Hospitals to Bypass CDC and Send Coronavirus Patient Information Directly to Washington Database Likely to Worsen Pandemic Response Rather than Improve It
(Washington, DC – July 15, 2020) — The U.S. Centers for Disease Control and Prevention (CDC), as the nation’s lead public health agency, is uniquely qualified to collect, analyze and disseminate information regarding infectious diseases. It has been serving in that role since its creation and, in close collaboration with U.S. healthcare facilities nationwide, has developed a health statistics infrastructure that is the gold standard worldwide.
The problems with regard to the COVID-19 data collection have largely been a result of the decentralized and fragmented nature of both healthcare and public health in the United States. Furthermore, hospital data is only one aspect of what we need to know to fight the pandemic. A key role of health departments at all levels of government is to aggregate data to produce a detailed picture of a health problem at the national, state and local levels. Inadequate funding for data infrastructure, at CDC and at the local, state, tribal and territorial levels, is also a contributing factor. That underfunding should be corrected rather than bypassed.
In the midst of the worst public health crisis in a century, it is counter-productive to create a new mechanism which will be extremely complicated to build and implement. Another area of concern is that the planning for this new approach did not substantively involve officials at the local, state, tribal and/or territorial levels. This is a time to support the public health system not take actions which may undermine its authority and critical role.
Americans must have confidence in the integrity of health data and its insulation from even the suggestion of political interference. Sending these sensitive data to a newly created entity overseen directly by the White House will not eliminate such concerns, it will increase them.
John Auerbach, President and CEO, Trust for America’s Health
Dr. Tom Frieden, President and CEO, Resolve to Save Lives
Lori T. Freeman, Chief Executive Officer, National Association of County and City Health Officials
Dr. Georges C. Benjamin, Executive Director, American Public Health Association
Thomas M. File, Jr., M.D., MSc, FIDSA; President, Infectious Disease Society of America
Chrissie Juliano, MPP, Executive Director, Big Cities Health Coalition
William H. Dietz, MD, PhD, Chair, Redstone Center for Prevention and Wellness, George Washington University
Nearly 350 Public Health Organizations Implore HHS Secretary Azar to Support CDC’s Critical Role in the COVID-19 Pandemic Response
Letter calls on Secretary Azar to “speak up” and be an advocate for CDC and public health
(Washington, DC – July 7, 2020) – The expertise of the U.S. Centers for Disease Control and Prevention (CDC) and all public health agencies is critical to protecting Americans’ health during the COVID-19 crisis, said a letter to Health and Human Services Secretary Alex Azar from 347 health and public health organizations released today.
The authoring organizations, including the American Public Health Association, Association of State and Territorial Health Officials, Big Cities Health Coalition, National Association of County and City Health Officials and Trust for America’s Health, expressed “deep concern” about increasing reports of resistance to evidence-based public health messages and threats to public health leaders and agencies, and called on the Secretary to be an advocate for public health.
At this sentinel moment, during the worst public health emergency in over a century, all of the nation’s leaders must resist any efforts that would undermine the critical role of the CDC to respond to the pandemic and must be an advocate for increased investment in public health, said the letter signatories.
“Secretary Azar, we urge you to speak up and amplify the critical role of CDC and that of all public health agencies during this monumental crisis,” the letter said.
The public health community’s work to respond to the pandemic, via the federal government, including within the CDC, and at the state, local, territorial and tribal levels, has been tireless but has been hamstrung by shrunken programs and inadequate technology; the result of decades of underfunding.
Public health leaders are calling attention to the need for CDC to play a central role as the nation’s navigates the COVID-19 pandemic, including:
“CDC is the world’s premier public health institution and should be treated as such during this pandemic. It must be appropriately funded and allowed to speak based on the best available science and with an unfettered voice,” said John Auerbach, President and CEO of Trust for America’s Health.
“When you look at the global response to the COVID-19 pandemic, countries that listen to and prioritize public health fare best,” said Dr. Tom Frieden, former director of the CDC, President and CEO of Resolve to Save Lives, an initiative of Vital Strategies. “Trying to fight this pandemic without daily, public guidance from the CDC is like fighting with one hand tied behind your back.”
“There’s no federal agency better suited to lead the response to this unprecedented pandemic. CDC has experts who have studied and helped control coronaviruses and other viral threats for decades, and can help our country emerge from this crisis,” said Dr. Julie Gerberding, former director of the CDC, Co-Chair CSIS Commission on Strengthening America’s Health Security.
The COVID-19 crisis has also illuminated the ways in which racial inequities impact health. Higher rates of COVID-19 deaths within communities of color illustrate the importance of all of CDC’s work, including its focus on chronic disease prevention. It is not possible to effectively meet the needs of the American people if that scope is narrowed.
The letter furthermore calls on Secretary Azar to be an advocate for increased funding for CDC’s core budget. While emergency supplemental funding has been critical to begin to address the immediate COVID-19 response needs, robust, sustained, and predictable funding for its full public health mission is essential to sustain its public health activities and to prevent the next emergency. Increasing the federal investment in public health will be particularly important, as state and local government budgets are likely to be severely hampered in the coming fiscal year due to tax revenue losses during the COVID-19 related economic shutdown.
Today’s laser focus should be on preventing further deaths and disruptions due to the pandemic and the CDC, as the world’s premier public health institution, should be at the helm of that effort, the letter said. Once the pandemic is controlled, the CDC, other federal agencies, state and local leaders and the public health community should collaboratively evaluate their performance and must acknowledge and address shortcomings of the response in order to be better prepared for the next public health emergency.
Signing the letter were:
1,000 Days
Academic Health Resource
Academy for Eating Disorders
Action on Smoking and Health
Advocates for Better Children’s Diets
AES Consulting
AFSCME
AIDS Alliance for Women, Infants, Children, Youth & Families
AIDS United
AlohaCare
Alzheimer’s and Dementia Alliance of WI
Alzheimer’s Association
Alzheimer’s Impact Movement (AIM)
Alzheimer’s of Central Alabama
Alzheimer’s Orange County
American Academy of Family Physicians
American Academy of Pediatrics
American Academy of Pediatrics, California
American Association for Clinical Chemistry
American Association for Dental Research
American Association for the Study of Liver Diseases
American Association of Colleges of Pharmacy
American Association on Health and Disability
American Cancer Society Cancer Action Network (ACS CAN)
American College Health Association
American College of Clinical Pharmacy
American College of Clinical Pharmacy (ACCP)
American College of Obstetricians and Gynecologists
American College of Physicians
American College of Preventive Medicine
American Council on Exercise
American Dental Association
American Foundation for Suicide Prevention
American Geriatrics Society
American Heart Association
American Kidney Fund
American Lung Association
American Medical Women’s Association
American Organization for Nursing Leadership
American Public Health Association
American School Health Association
American Sexual Health Association
American Society for Clinical Pathology
American Society for Microbiology
American Society of Hematology
American Society of Pediatric Nephrology
American Society of Tropical Medicine & Hygiene
American Thoracic Society
American University Department of Health Studies
APLA Health
Arizona Community Health Workers Association
Arizona Public Health Association
Art & Science of Health Promotion Institute
Asian Health Coalition
Asian Health Services
Association for Prevention Teaching and Research
Association for Professionals in Infection Control and Epidemiology
Association of American Cancer Institutes
Association of American Medical Colleges
Association of Asian Pacific Community Health Organizations (AAPCHO)
Association of Departments of Family Medicine
Association of Family Medicine Residency Directors
Association of Food and Drug Officials
Association of Immunization Managers
Association of Maternal & Child Health Programs
Association of Minority Health Professions Schools
Association of Ohio Health Commissioners
Association of Population Centers
Association of Public Health Laboratories
Association of Schools and Programs of Public Health
Association of SNAP Nutrition Education Administrators
Association of State and Territorial Health Officials
Association of State Public Health Nutritionists
Autistic Self Advocacy Network
Big Cities Health Coalition
Bipartisan Policy Center
Black AIDS Institute
Black Men’s Health Initiative
Boston Public Health Commission
Bristol Health Equity Zone
Bronx Health REACH
California Coalition for Children’s Safety and Health
California Immunization Coalition
California Pan-Ethnic Health Network
California School Nurses Organization
Cambridge Public Health Department
Campaign for Tobacco-Free Kids
Cancer Council of the Pacific Islands
Caring Ambassadors Program
Cascade AIDS Project
Center for Community Resilience
Center for Health and Learning
Center for Law and Social Policy (CLASP)
CenterLink: The Community of LGBT Centers
Ceres Community Project
ChangeLab Solutions
Child Welfare League of America
Children’s Environmental Health Network
Children’s Mental Health Network
Christian Council of Delmarva
City of Houston Health Department
City of Milwaukee of Health Department
Climate for Health, ecoAmerica
Coalition for a Tobacco Free Arkansas
Coalition of National Health Education Organizations
Cohen Veterans Bioscience
Colorado Association of Local Public Health Officials
Colorado Public Health Association
Colorado Public Health Nursing Leaders
Community Access National Network
Community Education Group
Connecticut Public Health Association
Cooley’s Anemia Foundation
Council of State and Territorial Epidemiologists
Counter Tools
County Health Executives Association of California
Cuyahoga County Board of Health
Cystic Fibrosis Foundation
Delaware Academy of Medicine
Delaware Academy of Medicine / Delaware Public Health Association
Delaware Academy of Medicine and the Delaware Public Health Association
East Shore District Health Dept.
Eating Disorders Coalition for Research, Policy & Action
Education Development Center
Element Health, Inc.
Endocrine Society
Enlace Chicago
Epilepsy Alliance America
Epilepsy Foundation
Equality California
Eta Sigma Gamma
Families USA
Family Voices
Fetal Alcohol Syndrome Information Network
FHI 360
FIRST Family Service Center
Fletcher Group, Inc.
Florida Institute for Health Innovation
Florida Public Health Association
Foundation for Healthy Generations
Galaxy Aviation Corp
Gateway Region YMCA
George Mason University Center for Climate Change Communication
GLMA: Health Professionals Advancing LGBTQ Equality
Global Alliance for Behavioral Health and Social Justice
Global Health Council
Global Health Technologies Coalition (GHTC)
Global Healthy Living Foundation
Global Liver Institute
Grand Traverse County Health Department
Green & Healthy Homes Initiative
Harm Reduction Michigan
Hawaii Public Health Association
Hawaii State Dept of Health, Office of Primary Care and Rural Health
Health by Design
Health Care Improvement Foundation
Health Enhancement Research Organization (HERO)
Health Resources in Action
Healthcare Foundation Northern Sonoma County
Healthcare Ready
HealthHIV
HealthPartners Institute
Healthy Schools Campaign
Healthy Weight Partnership Inc.
Heartland Alliance
Hep B United
Hepatitis B Foundation
HIV Medicine Association
Hogg Foundation for Mental Health
Hope and Help Center of Central Florida, Inc.
Idaho Public Health Association
Immunization Action Coalition
Immunize Nevada
Impetus – Let’s Get Started LLC
Indiana Public Health Association
Infectious Diseases Society of America
Institute for Family Health
Interdisciplinary Association for Population Health Science (IAPHS)
International Association of Emergency Managers
International Association of Fire Chiefs
IWC Resources, LP
Jeffrey Modell Foundation
Journal of Public Health Management and Practice
Jump IN for Healthy Kids
Kaplan Health Innovations
Kentucky Health Departments Association
KidsAndCars.org
L.A. Care Health Plan
Lakeshore Foundation
League of American Bicyclists
Linn County Public Health
Louisiana Community Health Worker Outreach Network
Louisiana Public Health Association
Lupus and Allied Diseases Association, Inc.
Macoupin County Public Health Department
Maine Public Health Association
March of Dimes
MaryCatherine Jones Consulting, LLC
Maryland Association of County Health Officers (MACHO)
Maryland Office of Minority Health
Massachusetts Public Health Association
Medicago
MEND Foundation
Metropolitan Group
Michigan Association for Local Public Health
MindWise Innovations
Minneapolis Health Department
Mississippi Public Health Institute
Montana Public Health Association
Monterey County Health Department
Morehouse School of Medicine
MountainCare
Multnomah County Health Department
NAACP
NAPHSIS
NASTAD
National Adult Day Services Association
National Association of Chronic Disease Directors
National Association of Community Health Workers
National Association of County and City Health Officials
National Association of Pediatric Nurse Practitioners
National Association of School Nurses
National Athletic Trainers’ Association
National Birth Equity Collaborative
National Center for Disaster Preparedness, Columbia University
National Center for Healthy Housing
National Coalition for LGBT Health
National Coalition for the Homeless
National Coalition of STD Directors
National Environmental Health Association (NEHA)
National Forum for Heart Disease & Stroke Prevention
National Hemophilia Foundation
National Kidney Foundation
National Lipid Association
National Medical Association (NMA)
National Network of Public Health Institutes
National Nurse-Led Care Consortium
National Prevention Science Coalition to Improve Lives
National REACH Coalition
National Safety Council
National Viral Hepatitis Roundtable
National WIC Association
Nebraska Association of Local Health Directors
Network for Environmental & Economic Responsibility of United Church of Christ
Nevada Public Health Organization
Nevada Rural Hospital Partners
New Jersey Association of County and City Health Officials
New Jersey Public Health Association
New York State Public Health Association
North American Primary Care Research Group
North Carolina Healthcare Foundation
Northwest Center for Public Health Practice
NYU Grossman School of Medicine
NYU School of Global Public Health
Ohio Public Health Association
Onyx Strategic Consulting LLC
Pacific Island Health Officers Association
Partnering for Community Transformation Inc
Partnership to Fight Chronic Disease
Partnership to Fight Infectious Disease
PATH
Patrick Risha CTE Awareness Foundation
Pawtucket Central Falls Health Equity Zone
Peggy Lillis Foundation
Pennsylvania Public Health Association
PFLAG National
Population Association of America
Population Health Alliance
Prevent Blindness
Prevent Child Abuse America
Prevention Institute
Preventive Cardiovascular Nurses Association
Public Health Advocates
Public Health Alliance of Southern California
Public Health Foundation
Public Health Institute
Public Health Law Center
Public Health Solutions
Puerto Rico Public Health Association
Pulmonary Hypertension Association
Redstone Global Center for Prevention and Wellness GWU
Research!America
Residential Eating Disorders Consortium
RESOLVE
Resolve to Save Lives, an initiative of Vital Strategies
Respiratory Health Association
Rhode Island Department of Health
RiverStone Health
Rural Health Association of Tennessee
Rural Health Association of Utah
Safe Routes Partnership
Safe States Alliance
Samueli Integrative Health Programs
SANIPLAN
School-Based Health Alliance
SF Hep B Free – Bay Area
SHAPE America – Society of Health and Physical Educators
Shoals Community Clinic
Silver State Equality-Nevada
Smoke Free St. Joe
Society for Advancement of Violence and Injury Research
Society for Maternal-Fetal Medicine
Society for Public Health Education
Society of State Leaders of Health and Physical Education
Society of Teachers of Family Medicine
Southern California Public Health Association
Southwick BOH
Stanislaus County Medical Society
Susan G. Komen
Tennessee Justice Center
Tennessee Public Health Association
Texas Public Health Association
The AIDS Institute
The Broussard Company
The Center for Community Resilience, George Washington University
The Consortium
The Foundation for Sustainable Communities
The George Washington University (GW) Cancer Center
The Gerontological Society of America
The Immunization Partnership
The John A. Hartford Foundation
The Kennedy Forum
The Los Angeles Trust for Children’s Health
The National Commission for Health Education Credentialing, Inc
The Nourished Principles, LLC
The Permanente Medical Group
Thomas Jefferson University
Training Resources Network, Inc.
Treatment Action Group
Trillium Health
Trust for America’s Health
Truth Initiative
U.S. Breastfeeding Committee
UCLA Fielding School of Public Health
UNC Gillings School of Global Public Health
United Ostomy Associations of America
United Way of Greenwood and Abbeville Counties
University of Washington Department of Global Health
University of Washington School of Nursing
University of Washington School of Public Health
University of Wisconsin Population Health Institute
USAgainstAlzheimer’s
Vaccinate Your Family
Washington State Association of Local Health Officials
Washington State Department of Health
Washington State Public Health Association
WelCore Health, LLC
West Valley Neighborhoods Coalition
Whitefoord
Winer Family Foundation
Wisconsin Public Health Association
Women Of A Certain Age
WomenHeart: The National Coalition for Women with Heart Disease
Women’s Resource Center
Woodhull Freedom Foundation
Xavier University for Population Health
YMCA of the USA
Zell Community Health Strategies
Sign-on Letter in Support of CDC Mission (July 2020)
Annual Deaths Due to Alcohol, Drugs or Suicide Exceeded 150,000 According to the Most Recent Data – And Could Get Worse Due to COVID-19
Alcohol, drug and suicide deaths up in 27 states
(Washington, DC – May 21, 2020) – Newly released data show that 151,964 Americans died due to alcohol, drugs or suicide in 2018. This 2018 national death rate for alcohol, drug and suicide deaths was only very slightly lower than what it had been in 2017 despite progress in reducing deaths due to some types of opioid overdose, according to a new study by Trust for America’s Health (TFAH) and Well Being Trust (WBT).
Between 2017 and 2018, 27 states experienced higher rates (increases above 0.04 percent) of alcohol, drug and suicide deaths. Two states, Vermont and Delaware, experienced double-digit death rate increases – 13 percent and 10 percent respectively. Twenty-three states and the District of Columbia had lower alcohol, drug and suicide deaths during the same period.
States with the highest alcohol, drugs and suicide death rates in 2018 were:
- West Virginia (84.9 per 100,000)
- New Mexico (82.8 per 100,000)
- New Hampshire (68.2 per 100,000)
- Alaska (67.8 per 100,000)
- Delaware (62.9 per 100,00)
States with the lowest alcohol, drug and suicide rates in 2018 were:
- Texas (31.7 per 100,000)
- Mississippi (31.7 per 100,000)
- Hawaii (34.6 per 100,000)
- Nebraska (35.5 per 100,000)
- Iowa (35.7 per 100,000)
For the year, alcohol deaths were up 4 percent and suicide deaths were up 2 percent across the country. The new data also show a continuing shift within the opioid crisis with reductions in deaths due to prescription opioid abuse but increases in deaths involving synthetic opioids including fentanyl. Death rates for all opioids were down 2 percent, but the death rate for synthetic opioids was up 10 percent. Additionally, heroin deaths were lower but deaths due to cocaine and psychostimulants abuse were higher.
While still disturbingly high, the 2018 data is the first time since 1999, when the current data collection began, that there hasn’t been a sizable increase in the national alcohol, drugs and suicide deaths per 100,000 rate. However, this stabilization in the deaths rate was not uniform. Some places and populations groups are experiencing stable or decreasing deaths rates while rates among other groups or in other places are continuing to rise.
“These data are a clarion call to action,” said John Auerbach, President and CEO of Trust for America’s Health. “We know what works to address deaths of despair but progress has been uneven and death rates continue to climb, with communities of color experiencing higher rates of increases in drug and alcohol deaths. And there’s another immediate concern: the COVID-19 crisis has increased the health burdens and economic pressures on many communities of color.”
American Indians, Asians, Blacks, Latinos and older adults all experienced increases in drug-induced deaths between 2017 and 2018. Blacks and American Indians had the largest increase. Blacks now have higher synthetic opioid overdose rates (10.7 per 100,000), cocaine overdose rates (8.8 per 100,000) and nearly the same overall drug-induced death rate (21.8 per 100,000) as Whites, after decades of having substantially lower overdose rates. Population groups that experienced lower drug-induced death rates in 2018 included adults ages 18-54 and Whites.
“Quite simply, too many Americans are dying from preventable causes. The profound racial health disparities seen in these data show that many ethnic minority groups are being left behind in our response efforts,” said Benjamin F. Miller, PsyD, chief strategy officer, Well Being Trust. “The nation needs a comprehensive framework for excellence in mental health and well-being, one that intentionally provides solutions for American Indians, Blacks, Asians and Latinos. With all the other COVID-19 related investments, it’s time for the federal government to fully invest in mental health now and for all states to take action.”
Deaths by Drug Type
Synthetic Opioids – in 2018, 31,355 Americans died from synthetic opioid overdose; up 10 percent since 2017. In total, the synthetic-opioid-involved overdose death rate has increased 10-fold since 2013.
Cocaine – In 2018, 14,666 Americans died from cocaine-involved overdoses; up 5 percent since 2017. The overall cocaine overdose death rate has increased by 187 percent since 2013.
Other psychostimulants – In 2018, 12,676 Americans died from overdoses involving psychostimulants and 52,279 have died over the past decade due to psychostimulants abuse. The 2018 psychostimulants overdose death rate was 22 percent higher than it was in 2017.
Alcohol-induced Deaths
In 2018, 37,329 Americans died due to alcohol-induced causes; the rate of alcohol-induced deaths in 2018 was 4 percent higher than the prior year.
Alcohol induced deaths are highest among American Indians (30.0 per 100,000) and adults ages 55 to 74 (27.6 per 100,000). All population groups had higher rates of alcohol deaths in 2018 as compared to the prior year except youths ages 0-17, whose rate held steady.
Suicide Deaths
In 2018, 48,344 Americans died as a result of suicide. Nationally, the 2018 suicide rate was two percent higher than the prior year (that is after a four percent increase in 2017). Suicide rates increased across all demographics, except for adults ages 18-54 whose rate remained stable. In addition, all racial and ethnic minority groups experienced larger proportional changes in suicide rates than did Whites.
Death by suicide in 2018 was highest among males (23.4 percent per 100,000), those living in rural areas (19.7 per 100,000), Whites (16.8 per 100,000) and American Indian/Alaska Natives (14.1 per 100,000).
# # #
Trust for America’s Health is a nonprofit, nonpartisan organization that promotes optimal health for every person and community and makes the prevention of illness and injury a national priority. www.tfah.org. Twittwe: @HealthyAmerica1
Well Being Trust is a national foundation dedicated to advancing the mental, social, and spiritual health of the nation. Created to include participation from organizations across sectors and perspectives, Well Being Trust is committed to innovating and addressing the most critical mental health challenges facing America, and to transforming individual and community well-being. www.wellbeingtrust.org. Twitter: @WellBeingTrust
Comments on USDA Proposed Rule Change to National School Lunch and Breakfast Programs (April 2020)
New Report Places 25 States and DC in High Performance Tier on 10 Public Health Emergency Preparedness Measures
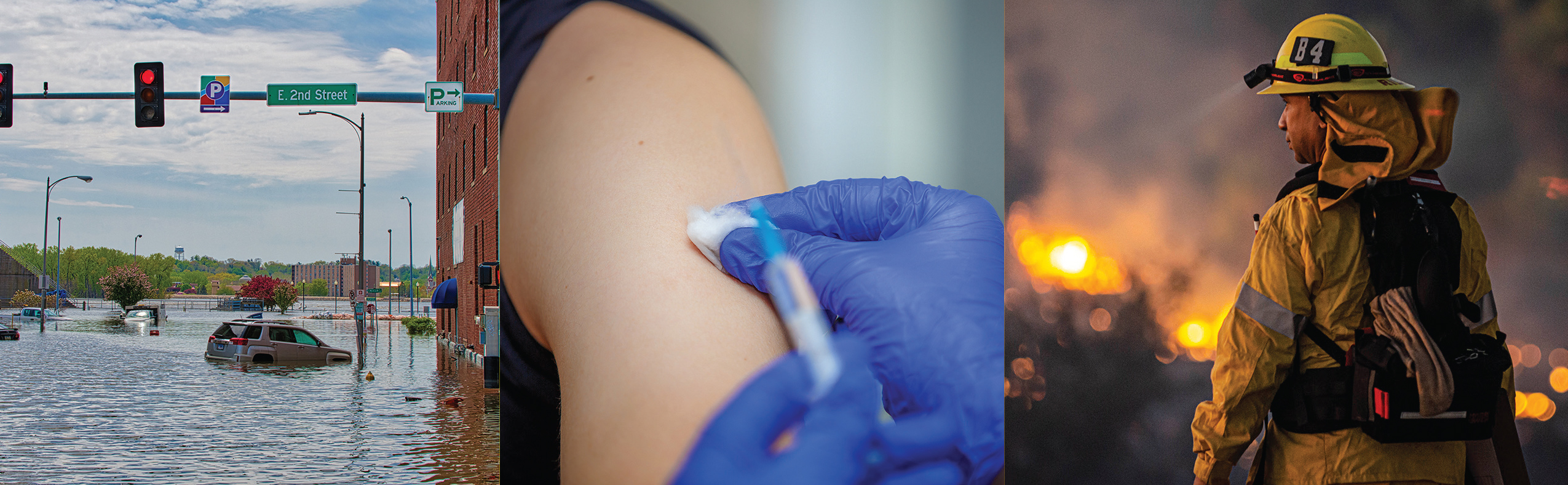
As Threats Increase, Annual Assessment Finds States’ Level of Readiness for Health Emergencies is Improving in Some Areas but Stalled in Others
February 5, 2020
(Washington, DC) – Twenty-five states and the District of Columbia were high-performers on a three-tier measure of states’ preparedness to protect the public’s health during an emergency, according to a new report released today by Trust for America’s Health (TFAH). The annual report, Ready or Not 2020: Protecting the Public’s Health from Diseases, Disasters, and Bioterrorism, found year-over-year improvement among 10 emergency readiness measures, but also notes areas in need of improvement. Last year, 17 states ranked in the report’s top tier.
For 2020, 12 states placed in the middle performance tier, down from 20 states and the District of Columbia in the middle tier last year, and 13 placed in the low performance tier, the same number as last year.
The report found that states’ level of preparedness has improved in key areas, including public health funding, participation in healthcare coalitions and compacts, hospital safety, and seasonal flu vaccination. However, other key health security measures, including ensuring a safe water supply and access to paid time off, stalled or lost ground.
| Performance Tier | States | Number of States |
| High Tier | AL, CO, CT, DC, DE, IA, ID, IL, KS, MA, MD, ME, MO, MS, NC, NE, NJ, NM, OK, PA, TN, UT, VA, VT, WA, WI |
25 states and DC |
| Middle Tier | AZ, CA, FL, GA, KY, LA, MI, MN, ND, OR, RI, TX | 12 states |
| Low Tier | AK, AR, HI, IN, MT, NH, NV, NY, OH, SC, SD, WV, WY | 13 states |
The report measures states’ performance on an annual basis using 10 indicators that, taken together, provide a checklist of a jurisdiction’s level of preparedness to prevent and respond to threats to its residents’ health during an emergency. The indicators are:
| Preparedness Indicators | |||
| 1 | Incident Management: Adoption of the Nurse Licensure Compact. | 6 | Water Security: Percentage of the population who used a community water system that failed to meet all applicable health-based standards. |
| 2 | Cross-Sector Community collaboration: Percentage of hospitals participating in healthcare coalitions. | 7 | Workforce Resiliency and Infection Control: Percentage of employed population with paid time off. |
| 3 | Institutional Quality: Accreditation by the Public Health Accreditation Board. | 8 | Countermeasure Utilization: Percentage of people ages 6 months or older who received a seasonal flu vaccination. |
| 4 | Institutional Quality: Accreditation by the Emergency Management Accreditation Program. | 9 | Patient Safety: Percentage of hospitals with a top-quality ranking (“A” grade) on the Leapfrog Hospital Safety Grade. |
| 5 | Institutional Quality: Size of the state public health budget, compared with the past year. | 10 | Health Security Surveillance: The public health laboratory has a plan for a six-to eight-week surge in testing capacity. |
Four states (Delaware, Pennsylvania, Tennessee, and Utah) moved from the low performance tier in last year’s report to the high tier in this year’s report. Six states (Illinois, Iowa, Maine, New Mexico, Oklahoma, Vermont) and the District of Columbia moved up from the middle tier to the high tier. No state fell from the high to the low tier but six moved from the middle to the low tier. Hawaii, Montana, Nevada, New Hampshire, South Carolina, and West Virginia.
“The increasing number of threats to Americans’ health in 2019, from floods to wildfires to vaping, demonstrate the critical importance of a robust public health system. Being prepared is often the difference between harm or no harm during health emergencies and requires four things: planning, dedicated funding, interagency and jurisdictional cooperation, and a skilled public health workforce,” said John Auerbach, President and CEO of Trust for America’s Health.
“While this year’s report shows that, as a nation, we are more prepared to deal with public health emergencies, we’re still not as prepared as we should be. More planning and investment are necessary to saves lives,” Auerbach said.
TFAH’s analysis found that:
- A majority of states have plans in place to expand healthcare capacity in an emergency through programs such as the Nurse Licensure Compact or other healthcare coalitions. Thirty-two states participated in the Nurse Licensure Compact, which allows licensed nurses to practice in multiple jurisdictions during an emergency. Furthermore, 89 percent of hospitals nationally participated in a healthcare coalition, and 17 states and the District of Columbia have universal participation meaning every hospital in the state (+DC) participated in a coalition. In addition, 48 states and DC had a plan to surge public health laboratory capacity during an emergency.
- Most states are accredited in the areas of public health, emergency management, or both. Such accreditation helps ensure that necessary emergency prevention and response systems are in place and staffed by qualified personnel.
- Most people who got their household water through a community water system had access to safe water. Based on 2018 data, on average, just 7 percent of state residents got their household water from a community water system that did not meet applicable health standards, up slightly from 6 percent in 2017.
- Seasonal flu vaccination rates improved but are still too low. The seasonal flu vaccination rate among Americans ages 6 months and older rose from 42 percent during the 2017-2018 flu season to 49 percent during the 2018-2019 season, but vaccination rates are still well below the 70 percent target established by Healthy People 2020.
- In 2019, only 55 percent of employed people had access to paid time off, the same percentage as in 2018. The absence of paid time off has been shown to exacerbate some infectious disease outbreaks . It can also prevent people from getting preventive care.
- Only 30 percent of hospitals, on average, earned top patient safety grades, up slightly from 28 percent in 2018. Hospital safety scores measure performance on such issues as healthcare associated infection rates, intensive-care capacity and an overall culture of error prevention. Such measures are critical to patient safety during infectious disease outbreaks and are also a measure of a hospital’s ability to perform well during an emergency.
The report includes recommended policy actions that the federal government, states and the healthcare sector should take to improve the nation’s ability to protect the public’s health during emergencies.
Other sections of the report describe how the public health system was critical to the vaping crisis response, how health inequities put some communities at greater risk during an emergency, and the needs of people with disabilities during an emergency.
Read the full text report |
Ready or Not 2020: Protecting the Public’s Health from Diseases, Disasters and Bioterrorism
The State of Obesity 2019 Congressional Briefing: Better Policies for a Healthier America
On November 18th, 2019, Trust for America’s Health held a briefing for congressional staff and partners that reviewed the latest obesity rates and trends, the role of public health and other stakeholders in preventing, treating and responding to obesity and its comorbidities, highlighted promising approaches to ensure healthy communities, and offered evidence-based policy recommendations that could help all Americans lead healthier lives.
Briefing speakers included:
- John Auerbach, MBA, President and CEO, Trust for America’s Health
- Devita Davison, Executive Director, FoodLab Detroit
- Martha Halko, MS, RD, LD, Deputy Director of Prevention & Wellness, Cuyahoga County (Ohio) Board of Health
- Ruth Petersen, MD, MPH, Director, Division of Nutrition, Physical Activity, and Obesity, Centers for Disease Control & Prevention (CDC)
Briefing materials:
- Panelists biographies
- Presentation slides
- CDC Division of Nutrition, Physical Activity, and Obesity At A Glance fact sheet
- CDC Division of Nutrition, Physical Activity, and Obesity’s Work in Healthcare Settings to Reduce Childhood Obesity fact sheet
- TFAH’s State of Obesity 2019 Report
- TFAH’s State of Obesity 2019 report fact sheet
- Robert Wood Johnson Foundation’s (RWJF) 2019 Obesity Report
For more information, please contact Daphne Delgado, TFAH Senior Government Relations Manager at [email protected]